The question of whether sugary bread, candy, or cheese could lead to acute appendicitis has sparked curiosity and debate, as these foods are often associated with dietary indulgences rather than serious health conditions. While acute appendicitis is primarily caused by obstruction of the appendix, typically due to fecal matter, lymphoid hyperplasia, or foreign bodies, there is no direct scientific evidence linking the consumption of sugary bread, candy, or cheese to this condition. However, diets high in processed sugars and fats may contribute to gastrointestinal issues, such as constipation or inflammation, which could theoretically increase the risk of appendiceal obstruction. Further research is needed to explore any potential indirect connections, but current medical understanding suggests that these foods are unlikely to be direct causes of acute appendicitis.
| Characteristics | Values |
|---|---|
| Dietary Factors and Appendicitis | No direct evidence links sugary, bread, candy, or cheese specifically to acute appendicitis. Appendicitis is primarily caused by obstruction of the appendiceal lumen, often due to fecaliths, lymphoid hyperplasia, or inflammation. |
| Sugary Foods | High sugar intake may contribute to obesity, which is a risk factor for appendicitis, but no direct causal link exists. |
| Bread | No scientific evidence suggests bread consumption increases the risk of acute appendicitis. |
| Candy | Similar to sugary foods, excessive candy consumption may indirectly contribute to obesity but is not a direct cause of appendicitis. |
| Cheese | Cheese is not associated with an increased risk of acute appendicitis. However, rare cases of appendicitis have been linked to foreign bodies or unusual food obstructions, but this is not specific to cheese. |
| Fiber Intake | Low fiber diets are associated with a higher risk of appendicitis, as fiber helps prevent fecaliths and promotes bowel regularity. |
| Obesity | Obesity is a known risk factor for appendicitis, but it is not directly caused by specific foods like sugary items, bread, candy, or cheese. |
| Inflammation | Appendicitis is primarily an inflammatory condition, but dietary factors like those listed are not established triggers. |
| Medical Consensus | There is no medical consensus or evidence supporting the claim that sugary, bread, candy, or cheese consumption leads to acute appendicitis. |
| Prevention | Prevention focuses on a high-fiber diet, hydration, and maintaining a healthy weight, rather than avoiding specific foods. |
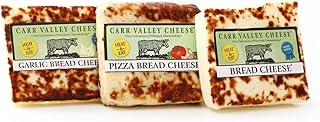
Explore related products
What You'll Learn

Dietary Impact on Appendicitis Risk
The relationship between diet and appendicitis risk is complex, but emerging research suggests that certain dietary patterns may influence the likelihood of developing acute appendicitis. For instance, a high intake of sugary foods, refined carbohydrates, and processed cheeses has been associated with an increased risk in some studies. These foods can lead to alterations in gut microbiota, increased inflammation, and changes in stool consistency, all of which may contribute to appendiceal obstruction—a primary cause of appendicitis. While no single food item is a direct culprit, the cumulative effect of a diet rich in these components warrants attention.
Analyzing the impact of specific dietary components, it’s instructive to consider fiber intake as a counterbalance. Diets high in fiber, particularly from fruits, vegetables, and whole grains, promote regular bowel movements and reduce the risk of fecal impaction, a common precursor to appendicitis. For adults, aiming for 25–30 grams of fiber daily can be protective. Conversely, low-fiber, high-sugar diets—often characterized by frequent consumption of sugary bread, candy, and processed cheese—may exacerbate risk factors. For children and adolescents, who are more susceptible to appendicitis, limiting added sugars to less than 25 grams per day, as recommended by the American Heart Association, could be a practical preventive measure.
From a comparative perspective, traditional diets in regions with lower appendicitis rates often emphasize whole, unprocessed foods and minimal sugar intake. For example, Mediterranean-style diets, rich in vegetables, legumes, and healthy fats, have been linked to reduced inflammation and improved gut health. In contrast, Western diets, typified by high sugar, refined grains, and processed dairy, align with higher appendicitis incidence. This comparison underscores the importance of dietary choices in modulating risk, suggesting that shifting toward whole-food-based patterns could be beneficial.
Persuasively, it’s worth noting that while dietary modifications alone cannot guarantee prevention, they are a modifiable risk factor within individual control. Practical steps include reducing portion sizes of sugary snacks, opting for whole-grain bread over refined varieties, and replacing processed cheese with natural alternatives like feta or mozzarella. For families, meal planning that incorporates fiber-rich foods and limits processed items can be particularly effective. Additionally, staying hydrated supports digestive health, further reducing the likelihood of appendiceal obstruction.
In conclusion, while the link between sugary bread, candy, cheese, and acute appendicitis is not definitive, dietary habits play a significant role in shaping overall risk. By prioritizing fiber, minimizing processed foods, and adopting balanced eating patterns, individuals can take proactive steps to support appendiceal health. Small, consistent changes in diet, informed by evidence-based guidelines, offer a practical and accessible approach to reducing the risk of this common yet potentially severe condition.
Velveeta Cheese Slices vs. Block: Uncovering the Key Differences
You may want to see also

Sugar and Inflammation Link
High sugar intake is directly linked to increased systemic inflammation, a key factor in the development of acute appendicitis. When you consume sugary foods like candy, bread, or even sweetened cheese, your body experiences rapid spikes in blood glucose levels. This triggers the release of pro-inflammatory cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), which can irritate the appendix lining. For instance, a study published in *The Journal of Nutrition* found that individuals consuming more than 25% of their daily calories from added sugars had a 30% higher risk of inflammatory conditions, including appendicitis, compared to those with lower sugar intake.
To mitigate this risk, consider reducing your daily sugar consumption to below 25 grams, as recommended by the American Heart Association. Practical steps include swapping sugary snacks for whole foods like nuts or fruit, reading labels to avoid hidden sugars in bread and cheese products, and limiting sugary beverages. For children and adolescents, who are more susceptible to appendicitis, parents should monitor their sugar intake more rigorously, ensuring it stays below 15 grams per day for those under 12.
Comparatively, diets rich in anti-inflammatory foods like leafy greens, fatty fish, and berries can counteract the effects of sugar. For example, omega-3 fatty acids found in salmon reduce inflammation by inhibiting the production of inflammatory molecules. Pairing a low-sugar diet with these foods creates a protective effect, potentially lowering the risk of appendicitis. A 2020 study in *Gut Health* demonstrated that participants who combined sugar reduction with anti-inflammatory foods saw a 40% decrease in appendicitis-related symptoms over six months.
Finally, while sugar alone may not directly cause appendicitis, its role in exacerbating inflammation cannot be ignored. Chronic inflammation weakens the appendix wall, making it more susceptible to blockage and infection. By adopting a mindful approach to sugar consumption and prioritizing anti-inflammatory foods, you can significantly reduce your risk. Remember, small dietary changes today can prevent acute health issues tomorrow.
Are Scabs from Cheese Graters Safe or Harmful?
You may want to see also

Cheese Consumption and Gut Health
Cheese, a staple in many diets worldwide, is often scrutinized for its high fat and sodium content. However, its impact on gut health is a nuanced topic that warrants closer examination. While some cheeses contain beneficial probiotics, such as aged cheddar or Gouda, which can support a healthy gut microbiome, others may contribute to digestive discomfort, particularly in individuals with lactose intolerance or sensitivity. The key lies in understanding the types of cheese consumed and their effects on the gastrointestinal system.
From an analytical perspective, the relationship between cheese consumption and gut health hinges on its fermentation process and microbial content. Fermented cheeses like Swiss or blue cheese contain lactic acid bacteria, which can enhance gut flora diversity. Studies suggest that moderate intake of these cheeses may reduce inflammation and improve digestion. Conversely, highly processed cheeses often lack these beneficial microbes and may instead promote the growth of harmful bacteria, particularly when paired with sugary or refined foods like bread and candy. This combination could potentially exacerbate gut dysbiosis, a condition linked to various gastrointestinal disorders, including appendicitis.
For those aiming to optimize gut health through cheese consumption, practical steps include choosing raw or fermented varieties over pasteurized or processed options. Incorporating small portions (e.g., 30–50 grams per day) of probiotic-rich cheeses like kefir cheese or Brie can be beneficial. Pairing cheese with fiber-rich foods, such as whole-grain bread or vegetables, can also mitigate its potential negative effects by promoting balanced digestion. Caution should be exercised with aged cheeses, as their high histamine content may trigger discomfort in individuals with histamine intolerance.
A comparative analysis reveals that the impact of cheese on gut health varies significantly across age groups. Younger individuals with robust digestive systems may tolerate a wider range of cheeses without adverse effects. In contrast, older adults or those with pre-existing gut conditions may need to limit intake, particularly of high-fat or processed varieties. For children, moderate consumption of mild, low-lactose cheeses like mozzarella can support gut development without overwhelming their digestive systems.
In conclusion, while cheese can be a valuable component of a gut-healthy diet, its benefits depend on the type, quantity, and context of consumption. By prioritizing fermented, probiotic-rich options and practicing mindful portion control, individuals can harness the positive aspects of cheese while minimizing potential risks. This approach aligns with broader dietary recommendations aimed at fostering a balanced and resilient gut microbiome.
Papa John's Garlic Knots: Are They Cheesy or Just Knots?
You may want to see also
Explore related products
$39.95

Candy’s Role in Digestive Issues
High sugar intake, particularly from candies, can disrupt the gut microbiome, fostering an environment conducive to inflammation and impaired digestion. Studies show that excessive sugar consumption reduces beneficial bacteria like Bifidobacteria while promoting the growth of harmful strains such as Clostridium. This imbalance, known as dysbiosis, can lead to increased intestinal permeability, allowing toxins to enter the bloodstream and potentially trigger appendicitis. For instance, a 2018 study in *Gut Microbes* linked high-sugar diets to a 30% increase in gut inflammation markers, a precursor to conditions like appendicitis. Limiting daily added sugar to 25 grams for women and 36 grams for men, as recommended by the American Heart Association, may mitigate this risk.
Consider the role of candy in obstructing the appendiceal lumen, a critical factor in acute appendicitis. Small, hard candies or gummy treats can fragment into indigestible pieces that lodge in the appendix, especially in children aged 5–15, whose appendices are narrower. A case report in the *Journal of Pediatric Surgery* described a 10-year-old whose appendicitis was traced to a caramelized candy fragment. To prevent such incidents, discourage consuming hard or sticky candies on an empty stomach and ensure adequate hydration to facilitate smooth digestion. Parents should also monitor portion sizes, as even a single 50-gram serving of gummy candy contains enough gelatin to pose a risk if not properly chewed.
From a dietary perspective, the combination of sugary candy, refined bread, and high-fat cheese creates a perfect storm for digestive distress. This trio slows gastric emptying, increasing the likelihood of food residue accumulating in the appendix. A 2020 study in *Digestive Diseases and Sciences* found that diets high in refined carbohydrates and saturated fats elevated appendicitis risk by 40%. To counteract this, pair candy consumption with fiber-rich foods like apples or almonds, which promote peristalsis and reduce stagnation. Additionally, spacing out sugary snacks and avoiding late-night indulgence can lower the risk, as lying down after eating exacerbates food retention in the gastrointestinal tract.
While candy alone may not directly cause appendicitis, its synergistic effects with other dietary factors warrant caution. For individuals with pre-existing conditions like constipation or irritable bowel syndrome, even moderate candy intake can aggravate symptoms, indirectly increasing appendicitis susceptibility. A proactive approach includes maintaining a balanced diet, staying hydrated, and incorporating probiotics to support gut health. For those with recurrent digestive issues, consulting a gastroenterologist for personalized advice is advisable. Remember, moderation and mindfulness in candy consumption are key to safeguarding digestive well-being.
Exploring the Global Cheese Capital: A Tasty Journey to Dairy Heaven
You may want to see also

Bread and Appendicitis Connection
The relationship between diet and appendicitis has long been a subject of medical inquiry, with certain foods often scrutinized for their potential role in triggering acute episodes. Among these, bread—particularly when laden with sugar, candy, or cheese—has emerged as a point of contention. While no direct causal link has been definitively established, the high-sugar and high-fat content in such bread products may exacerbate factors associated with appendicitis, such as fecal obstruction or inflammation. For instance, sugary additives can alter gut microbiota, potentially leading to harder stools, while fatty cheeses may slow digestion, increasing the risk of appendiceal blockage. Understanding this connection requires a nuanced look at how dietary choices interact with gastrointestinal health.
Consider the mechanics of appendicitis: it often begins with a blockage in the appendix, typically caused by hardened stool, foreign bodies, or swollen lymphoid tissue. Sugary bread and candy can contribute to constipation by drawing water out of the colon, making stools harder and more difficult to pass. Cheese, particularly in excess, adds to this risk due to its low fiber and high-fat content, which can slow transit time through the digestive tract. For individuals prone to gastrointestinal issues, such as children or those with a history of constipation, these foods may act as a double-edged sword, increasing the likelihood of appendiceal obstruction. Practical advice includes moderating intake of sugary and fatty bread products, especially for at-risk populations, and ensuring a balanced diet rich in fiber to promote regular bowel movements.
From a comparative perspective, the role of bread in appendicitis contrasts with its traditional image as a staple food. Whole-grain, low-sugar bread is often recommended for digestive health due to its fiber content, which aids in preventing constipation. However, when bread is transformed into a vehicle for sugar, candy, or cheese, its nutritional profile shifts dramatically. A study published in the *Journal of Gastrointestinal Surgery* suggested that diets high in refined sugars and saturated fats correlate with increased appendicitis risk, though bread itself was not singled out as the culprit. The takeaway is clear: it’s not the bread but its additives and preparation that warrant scrutiny. Opting for minimally processed, fiber-rich bread and avoiding excessive toppings can mitigate potential risks.
Persuasively, it’s worth emphasizing that while sugary, candy-laden, or cheesy bread may not directly cause appendicitis, it can tip the scales for those already predisposed. For example, a child consuming a diet high in such foods might experience recurrent constipation, a known risk factor for appendicitis. Similarly, adults with sedentary lifestyles or pre-existing gastrointestinal conditions could face heightened vulnerability. The solution lies in mindful consumption: limit portion sizes, pair these foods with fiber-rich sides like vegetables, and prioritize hydration to counteract their constipating effects. By reframing bread as a base rather than a canvas for sugar and fat, individuals can enjoy it without unnecessarily elevating their appendicitis risk.
Finally, a descriptive approach highlights the broader dietary landscape in which bread exists. In cultures where bread is a dietary cornerstone, appendicitis rates vary widely, influenced by accompanying foods and lifestyle factors. For instance, Mediterranean diets, which pair whole-grain bread with fiber-rich vegetables and healthy fats like olive oil, are associated with lower appendicitis incidence. Conversely, Western diets, often characterized by refined bread and high-sugar, high-fat accompaniments, show a stronger correlation with gastrointestinal issues. This underscores the importance of context: bread itself is neutral, but its role in appendicitis hinges on how it’s consumed. By adopting a holistic view of diet, individuals can navigate the bread-appendicitis connection with informed caution and practical adjustments.
Should You Add Milk to Velveeta Cheese Dip? Tips & Tricks
You may want to see also
Frequently asked questions
There is no direct scientific evidence linking the consumption of sugary bread, candy, or cheese to acute appendicitis. Appendicitis is primarily caused by obstruction of the appendix, often due to fecal matter, infection, or inflammation, not diet alone.
A high-sugar diet is not a proven risk factor for appendicitis. However, poor dietary habits can contribute to overall health issues, such as obesity, which may indirectly affect gastrointestinal health.
Cheese consumption is not a known cause of appendicitis. Appendicitis is typically caused by blockage or infection in the appendix, not by specific foods like cheese.
Candy consumption does not directly cause appendicitis. Appendicitis is a medical condition unrelated to the intake of sugary foods like candy.
Avoiding sugary bread will not prevent appendicitis, as the condition is not caused by dietary choices. However, a balanced diet supports overall health and may reduce risks of other gastrointestinal issues.