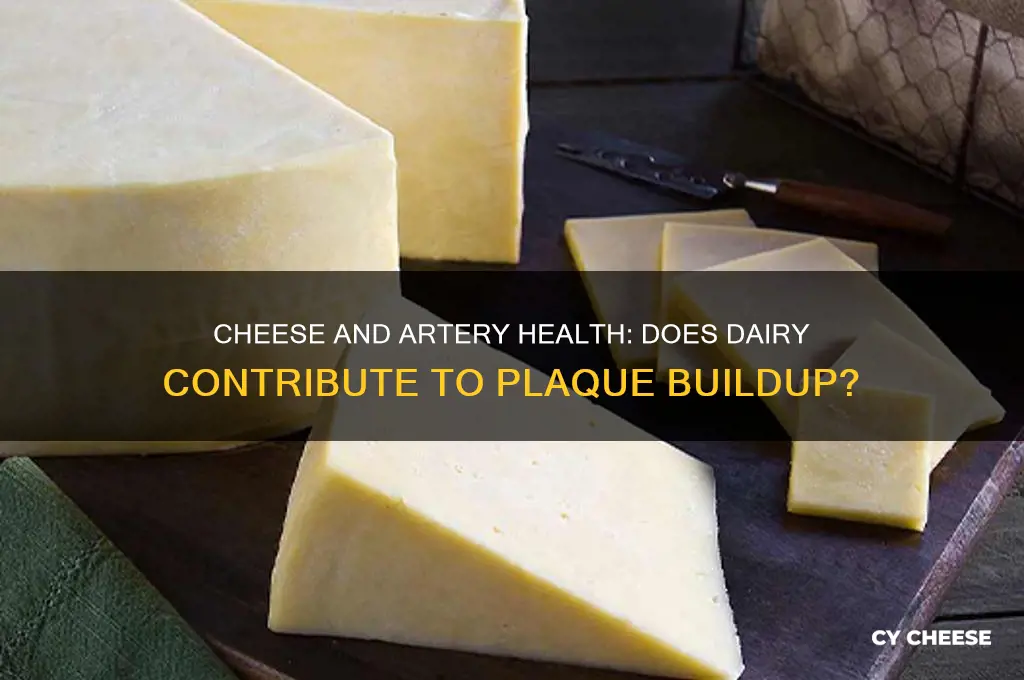
The question of whether cheese causes artery plaque is a topic of ongoing debate in the field of nutrition and cardiovascular health. Cheese, a beloved dairy product rich in saturated fats and cholesterol, has long been scrutinized for its potential role in atherosclerosis, the buildup of plaque in arteries. While some studies suggest that the saturated fats in cheese may contribute to elevated LDL (bad) cholesterol levels, a known risk factor for artery plaque, others argue that cheese contains beneficial nutrients like calcium, protein, and certain fatty acids that could mitigate its negative effects. Additionally, the impact of cheese on arterial health may vary depending on factors such as overall diet, portion size, and individual metabolism. As research continues to evolve, understanding the complex relationship between cheese consumption and artery plaque remains crucial for informed dietary choices.
| Characteristics | Values |
|---|---|
| Direct Causation | Cheese consumption alone does not directly cause artery plaque. Plaque buildup (atherosclerosis) is a complex process influenced by multiple factors, including diet, genetics, and lifestyle. |
| Saturated Fat Content | Cheese is high in saturated fat, which can raise LDL ("bad") cholesterol levels, a risk factor for plaque formation when consumed in excess. |
| Type of Cheese | Low-fat or reduced-fat cheeses have less impact on cholesterol levels compared to full-fat varieties. |
| Portion Size | Moderate consumption of cheese (e.g., 1-2 servings per day) is less likely to contribute to plaque buildup compared to excessive intake. |
| Overall Diet | Cheese consumed as part of a balanced diet (rich in fruits, vegetables, whole grains, and lean proteins) may mitigate its potential negative effects on arterial health. |
| Individual Variability | Genetic predisposition, metabolism, and existing health conditions (e.g., diabetes, hypertension) influence how cheese affects cholesterol and plaque risk. |
| Calcium and Protein | Cheese contains calcium and protein, which may have protective effects on heart health when consumed in moderation. |
| Processed vs. Natural Cheese | Processed cheeses often contain additional sodium and additives, which may worsen cardiovascular risk compared to natural cheeses. |
| Current Research | Recent studies suggest that moderate cheese consumption does not significantly increase the risk of cardiovascular disease or plaque buildup in healthy individuals. |
| Recommendations | Health guidelines advise limiting saturated fat intake (including from cheese) to <10% of daily calories to reduce plaque and heart disease risk. |
Explore related products
What You'll Learn

Dietary Fat Content in Cheese
Cheese, a staple in many diets worldwide, is often scrutinized for its fat content and potential role in cardiovascular health. The dietary fat in cheese, primarily saturated, has been a focal point in discussions about artery plaque formation. Saturated fats, which constitute about 60-70% of the fat in most cheeses, have historically been linked to elevated LDL cholesterol levels, a known risk factor for atherosclerosis. However, recent studies suggest a more nuanced relationship, emphasizing the importance of context—such as overall diet quality and individual metabolic responses—rather than singling out cheese as a culprit.
Analyzing the fat content in cheese reveals significant variability across types. For instance, a 30g serving of cheddar contains approximately 6g of fat, of which 4g is saturated, while the same portion of mozzarella contains around 4g of fat, with 3g saturated. Low-fat or part-skim options, like Swiss or feta, offer even lower fat profiles, making them viable alternatives for those monitoring fat intake. Understanding these differences allows consumers to make informed choices, balancing flavor preferences with health considerations.
From a practical standpoint, moderation and portion control are key when incorporating cheese into a heart-healthy diet. The American Heart Association recommends limiting saturated fat to no more than 5-6% of daily calories, which translates to about 13g for a 2,000-calorie diet. A single ounce of cheese can contribute significantly to this limit, so pairing it with fiber-rich foods like whole grains or vegetables can help mitigate its impact. For older adults or those with pre-existing cardiovascular conditions, consulting a dietitian to tailor cheese consumption to individual needs is advisable.
Comparatively, the fat in cheese is not inherently more harmful than other dietary fats when consumed mindfully. For example, replacing processed meats high in saturated and trans fats with cheese can be a healthier choice, as cheese also provides beneficial nutrients like calcium, protein, and vitamins. However, it’s critical to avoid compensating for cheese consumption by neglecting other aspects of a balanced diet. Overreliance on cheese as a protein source, for instance, could crowd out plant-based proteins that offer additional cardiovascular benefits.
In conclusion, the dietary fat content in cheese warrants attention but not alarm. By understanding the fat profiles of different cheeses, practicing portion control, and integrating cheese into a diverse and balanced diet, individuals can enjoy this food without undue concern about artery plaque. The key lies in viewing cheese as one component of a broader dietary pattern rather than isolating it as a singular risk factor.
Is Belvita Hot Mexican Cheese Discontinued? What We Know
You may want to see also

Saturated Fat and Heart Health
Cheese, a staple in many diets worldwide, often finds itself at the center of debates about heart health due to its saturated fat content. Saturated fats, commonly associated with animal products like cheese, have long been linked to increased levels of LDL cholesterol, a known risk factor for artery plaque buildup and cardiovascular disease. However, recent research suggests the relationship between saturated fat and heart health is more nuanced than previously thought. For instance, not all saturated fats behave identically in the body, and factors like overall diet quality, genetic predisposition, and lifestyle play significant roles in determining their impact.
To understand this better, consider the role of saturated fat in the context of a balanced diet. The American Heart Association recommends limiting saturated fat intake to no more than 5-6% of total daily calories. For someone consuming 2,000 calories per day, this equates to about 13 grams of saturated fat. A single ounce of cheddar cheese contains roughly 6 grams of saturated fat, which, when consumed in moderation, fits within these guidelines. The key lies in balancing cheese intake with other dietary choices, such as incorporating fiber-rich foods like vegetables, whole grains, and fruits, which can help mitigate the potential negative effects of saturated fat.
From a comparative perspective, not all cheeses are created equal in terms of saturated fat content. For example, part-skim mozzarella contains approximately 3 grams of saturated fat per ounce, making it a lower-fat alternative to cheddar or cream cheese. Opting for such varieties can allow individuals to enjoy cheese while adhering to heart-healthy dietary recommendations. Additionally, pairing cheese with foods rich in unsaturated fats, like nuts or avocado, can further support cardiovascular health by improving the overall lipid profile.
A persuasive argument for reevaluating the role of saturated fat in heart health comes from emerging studies that challenge traditional dietary guidelines. Some research suggests that replacing saturated fats with refined carbohydrates or sugars may not yield the expected cardiovascular benefits and could even be detrimental. Instead, focusing on whole, nutrient-dense foods—including moderate portions of cheese—within a Mediterranean-style diet has been associated with reduced risk of heart disease. This approach emphasizes the importance of dietary patterns over individual nutrients.
In practical terms, individuals concerned about saturated fat and artery plaque can adopt simple strategies to enjoy cheese while supporting heart health. For instance, portion control is crucial; limiting cheese servings to 1-2 ounces per day can help manage saturated fat intake. Pairing cheese with foods high in antioxidants, like berries or dark leafy greens, may also provide protective benefits. Finally, regular physical activity and maintaining a healthy weight are essential components of a holistic approach to cardiovascular wellness, complementing dietary choices to minimize the risk of plaque buildup.
Should Aged Gouda Be Refrigerated? Storage Tips for Optimal Flavor
You may want to see also

Cheese Consumption Studies
Cheese, a staple in diets worldwide, has long been scrutinized for its potential role in cardiovascular health, particularly in relation to artery plaque buildup. Recent studies have delved into the nuances of cheese consumption, revealing that not all cheeses—or consumption patterns—are created equal. For instance, a 2019 study published in the *European Journal of Nutrition* found that moderate intake of hard cheeses, such as cheddar or parmesan, did not significantly increase LDL cholesterol levels in healthy adults when consumed as part of a balanced diet. This challenges the blanket assumption that cheese universally contributes to arterial plaque.
Analyzing the data further, researchers have identified that the type of fat in cheese plays a critical role. Cheese contains both saturated and unsaturated fats, but the latter, particularly in fermented varieties like Swiss or Gouda, may counteract some of the negative effects of saturated fats. A study in the *American Journal of Clinical Nutrition* noted that participants who consumed 80 grams of cheese daily (equivalent to about three slices) showed no significant increase in arterial plaque markers compared to a control group. However, this finding was contingent on the absence of other high-saturated-fat foods in their diet, underscoring the importance of context in cheese consumption.
For those concerned about arterial health, practical tips emerge from these studies. First, portion control is key; limiting daily intake to 30–50 grams (roughly 1–2 ounces) aligns with findings that suggest minimal cardiovascular risk. Second, pairing cheese with fiber-rich foods like whole grains or vegetables can mitigate its impact on cholesterol levels. Lastly, age and pre-existing conditions matter—older adults or individuals with hypertension may need to further restrict cheese intake, as their bodies metabolize fats differently.
Comparatively, cheese fares better than other dairy products in some studies. For example, a 2020 meta-analysis in *Nutrients* found that butter consumption was more strongly correlated with increased arterial plaque than cheese, likely due to its higher concentration of saturated fats and lack of beneficial compounds like calcium and protein. This suggests that substituting butter with cheese in recipes could be a heart-healthier choice, though moderation remains paramount.
In conclusion, cheese consumption studies paint a nuanced picture. While excessive intake can contribute to arterial plaque, moderate consumption of certain types of cheese, especially when balanced with other dietary components, may pose minimal risk. Tailoring intake based on age, health status, and dietary context allows individuals to enjoy cheese without undue concern, turning a potential health hazard into a manageable indulgence.
Anti-Inflammatory Cheese: Discover Dairy Options for a Healthier Diet
You may want to see also
Explore related products

Role of Cholesterol in Plaque
Cholesterol, a waxy, fat-like substance, plays a dual role in the body: essential for building cells and producing hormones, yet detrimental when accumulated in excess. In the context of artery plaque, cholesterol is a key player, particularly in its oxidized form. When low-density lipoprotein (LDL) cholesterol, often termed "bad" cholesterol, infiltrates the arterial walls, it undergoes oxidation, triggering an inflammatory response. This process attracts immune cells, which engulf the oxidized LDL, transforming into foam cells. These foam cells accumulate, forming the core of atherosclerotic plaque, a hardened deposit that narrows and stiffens arteries. Understanding this mechanism is crucial, as it highlights how cholesterol directly contributes to plaque buildup, increasing the risk of heart disease and stroke.
To mitigate this risk, monitoring cholesterol levels is paramount. The American Heart Association recommends adults aged 20 and older have their cholesterol checked every 4–6 years. Optimal levels include LDL below 100 mg/dL and high-density lipoprotein (HDL) above 60 mg/dL. For those with a family history of heart disease or other risk factors, more frequent testing and stricter targets may be advised. Dietary modifications, such as reducing saturated and trans fats, can lower LDL levels. For instance, replacing butter with olive oil or limiting red meat intake can significantly impact cholesterol profiles. Statins, a class of medications, are often prescribed for individuals with LDL levels above 190 mg/dL or those at high cardiovascular risk, effectively reducing LDL by 20–60%.
Comparatively, not all cholesterol is harmful. HDL cholesterol acts as a scavenger, transporting LDL from the arteries to the liver for excretion. This protective role underscores the importance of balancing cholesterol types rather than eliminating it entirely. Lifestyle factors, such as regular aerobic exercise, can elevate HDL levels. For example, 150 minutes of moderate-intensity exercise weekly, like brisk walking or cycling, has been shown to increase HDL by 5–10%. Conversely, smoking and excessive alcohol consumption can lower HDL, exacerbating plaque formation. Thus, a holistic approach to cholesterol management, combining diet, exercise, and medication when necessary, is essential for preventing arterial plaque.
A practical takeaway is the impact of dietary choices on cholesterol levels. Cheese, often high in saturated fat, can elevate LDL cholesterol, particularly when consumed in excess. A single ounce of cheddar cheese contains approximately 6 grams of saturated fat, nearly one-third of the daily recommended limit for a 2,000-calorie diet. However, not all cheeses are equal; opting for low-fat varieties like mozzarella or feta can reduce saturated fat intake. Pairing cheese with fiber-rich foods, such as whole-grain crackers or vegetables, can also mitigate its cholesterol-raising effects by slowing fat absorption. Moderation and mindful selection are key, as cheese can be part of a balanced diet without significantly contributing to arterial plaque when consumed thoughtfully.
In conclusion, cholesterol’s role in plaque formation is multifaceted, driven by the oxidation of LDL and subsequent inflammatory processes. By monitoring cholesterol levels, adopting heart-healthy habits, and making informed dietary choices, individuals can reduce their risk of atherosclerosis. While cheese can contribute to elevated LDL, its impact can be minimized through moderation and strategic consumption. This nuanced understanding empowers individuals to navigate dietary choices while safeguarding arterial health.
Discover Hidden Cheese Locations in Vampire Survivors: A Guide
You may want to see also

Impact of Fermented Dairy Products
Fermented dairy products, such as cheese, yogurt, and kefir, have been staples in human diets for millennia, yet their impact on arterial health remains a subject of debate. Unlike fresh dairy, fermentation transforms these products through microbial action, altering their nutrient profiles and potentially influencing how they affect the body. For instance, fermentation breaks down lactose into lactic acid, making these products more digestible for lactose-intolerant individuals. But does this process mitigate or exacerbate the risk of artery plaque formation?
Consider the role of saturated fats, often cited as a culprit in arterial plaque buildup. Cheese, a fermented dairy product, is high in saturated fats, which have been traditionally linked to elevated LDL cholesterol levels—a known risk factor for atherosclerosis. However, recent studies suggest that the relationship between saturated fats and heart health is more nuanced. Fermented dairy products contain bioactive peptides and beneficial bacteria that may counteract some of the negative effects of saturated fats. For example, certain strains of probiotics found in fermented dairy can reduce inflammation and improve lipid profiles, potentially lowering the risk of plaque accumulation.
To harness the benefits of fermented dairy while minimizing risks, moderation and mindful selection are key. Opt for low-fat or reduced-sodium varieties of cheese, and pair them with a diet rich in fruits, vegetables, and whole grains. For older adults or those with pre-existing cardiovascular conditions, limiting daily cheese intake to 30–50 grams (about 1–2 ounces) is advisable. Younger, healthier individuals may tolerate slightly higher amounts, but portion control remains essential. Incorporating other fermented dairy products like yogurt or kefir can also diversify microbial intake, supporting gut health and potentially reducing systemic inflammation.
A comparative analysis of fermented versus non-fermented dairy highlights the former’s advantages. While milk and cream provide essential nutrients, their lack of fermentation limits their ability to modulate cholesterol metabolism or enhance gut health. Fermented dairy, on the other hand, offers a synergistic blend of nutrients and bioactive compounds that may protect arterial walls. For instance, the fermentation process increases the availability of vitamin K2, a nutrient associated with reduced arterial calcification. This distinction underscores the importance of choosing fermented options when considering dairy’s role in cardiovascular health.
In practical terms, integrating fermented dairy into a heart-healthy diet requires balance and awareness. Start by replacing processed snacks with a small portion of aged cheese or a cup of plain yogurt. Experiment with kefir smoothies or use fermented dairy as a condiment rather than a main ingredient. For those monitoring cholesterol, combine fermented dairy with soluble fiber sources like oats or legumes to further optimize lipid levels. By approaching fermented dairy as part of a holistic dietary strategy, individuals can enjoy its unique benefits without compromising arterial health.
Quick Tips for Perfectly Heating Pancho's Cheese Dip Every Time
You may want to see also
Frequently asked questions
Cheese is high in saturated fat, which can raise LDL ("bad") cholesterol levels, a risk factor for artery plaque buildup. However, moderate consumption as part of a balanced diet may not directly cause plaque in everyone.
Low-fat cheese reduces saturated fat intake, which may lower LDL cholesterol and decrease the risk of artery plaque. However, other dietary and lifestyle factors also play a significant role.
Cheese tends to have more saturated fat than milk or yogurt, making it potentially more harmful to arteries. However, portion control and choosing lower-fat options can mitigate this risk.
Yes, cheese can be included in a heart-healthy diet when consumed in moderation, paired with fiber-rich foods, and balanced with unsaturated fats, whole grains, fruits, and vegetables.