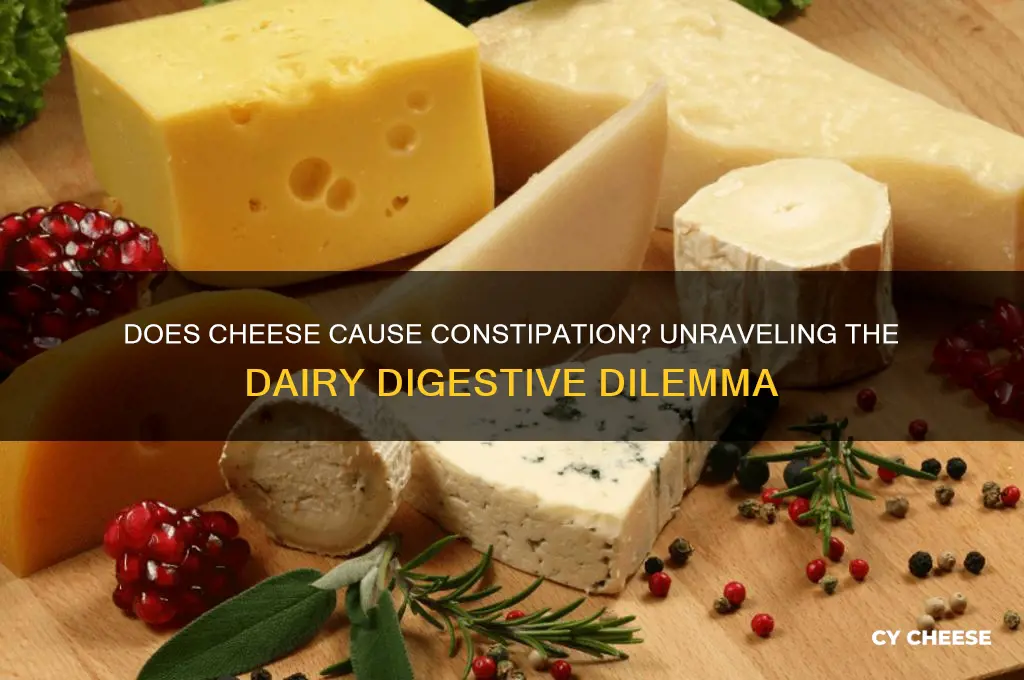
Cheese is a beloved food enjoyed worldwide, but its impact on digestion varies widely among individuals. Many people wonder whether cheese can cause constipation, a common digestive issue characterized by infrequent bowel movements or difficulty passing stool. Cheese is high in fat and low in fiber, two factors that can slow down digestion and potentially lead to constipation, especially when consumed in large quantities. Additionally, some individuals may be sensitive to lactose, a sugar found in dairy products, which can exacerbate digestive discomfort. However, the extent to which cheese contributes to constipation depends on factors such as the type of cheese, portion size, and an individual’s overall diet and digestive health. Understanding these variables can help determine whether cheese is a culprit in digestive issues or simply a harmless indulgence.
| Characteristics | Values |
|---|---|
| Does cheese cause constipation? | Cheese can contribute to constipation in some individuals, but it's not a universal effect. |
| Reason for potential constipation | High fat content, low fiber content, and individual lactose intolerance can slow down digestion and lead to constipation. |
| Types of cheese more likely to cause constipation | Hard cheeses (e.g., cheddar, parmesan) due to higher fat and lower moisture content. |
| Types of cheese less likely to cause constipation | Soft cheeses (e.g., mozzarella, ricotta) with higher moisture content. |
| Individual factors influencing constipation | Overall diet, hydration, physical activity, and pre-existing digestive conditions. |
| Recommended daily cheese intake | Moderation is key; 1-2 servings (1.5-2 oz) per day is generally considered safe for most people. |
| Alternatives for constipation-prone individuals | Low-fat cheeses, lactose-free cheeses, or plant-based cheese alternatives. |
| Importance of fiber and hydration | Increasing fiber intake and staying hydrated can help counteract constipation caused by cheese consumption. |
| Consultation with healthcare professional | If constipation persists or is severe, consult a doctor or dietitian for personalized advice. |
Explore related products
What You'll Learn
- Cheese and Lactose Intolerance: High lactose cheeses may cause constipation in lactose-intolerant individuals
- Hard vs. Soft Cheeses: Harder cheeses have less lactose, reducing constipation risk compared to softer types
- Fat Content Impact: High-fat cheeses can slow digestion, potentially leading to constipation in some people
- Fiber Pairing Tips: Eating cheese with fiber-rich foods can help prevent constipation and improve digestion
- Individual Sensitivity: Cheese affects everyone differently; monitor your body’s response to identify personal triggers

Cheese and Lactose Intolerance: High lactose cheeses may cause constipation in lactose-intolerant individuals
Cheese, a beloved staple in many diets, can sometimes lead to digestive discomfort, particularly for those with lactose intolerance. Lactose intolerance occurs when the body lacks sufficient lactase, the enzyme needed to break down lactose, a sugar found in milk and dairy products. While cheese is often considered a lower-lactose option compared to milk, certain varieties still contain enough lactose to trigger symptoms like bloating, gas, and constipation in sensitive individuals. High-lactose cheeses, such as fresh cheeses like ricotta, cottage cheese, and cream cheese, are more likely to cause issues. Understanding which cheeses to avoid or limit can help lactose-intolerant individuals enjoy dairy without discomfort.
Analyzing the lactose content in cheese reveals a wide range across types. Hard cheeses like cheddar, Parmesan, and Swiss undergo aging processes that break down much of their lactose, making them better tolerated. For example, a 1-ounce serving of cheddar contains less than 0.5 grams of lactose, while the same amount of cottage cheese can contain up to 3 grams. Soft, fresh cheeses retain more lactose because they are less processed. Lactose-intolerant individuals should opt for aged, hard cheeses and monitor portion sizes, as even small amounts of lactose can accumulate and cause symptoms if consumed throughout the day.
For those experiencing constipation from cheese, practical steps can alleviate discomfort. Start by identifying high-lactose cheeses in your diet and replace them with low-lactose alternatives. Pairing cheese with lactase supplements can also help break down lactose before it reaches the colon, reducing digestive symptoms. Staying hydrated is crucial, as water softens stool and aids bowel movements. Incorporating fiber-rich foods like fruits, vegetables, and whole grains can further promote regularity. If symptoms persist, consult a healthcare provider to rule out other conditions and discuss personalized dietary adjustments.
Comparing cheese to other dairy products highlights its unique role in lactose intolerance management. While milk and ice cream are often avoided due to their high lactose content, cheese is frequently overlooked as a culprit. However, its lactose content varies significantly, making it both a potential problem and a solution. For instance, lactose-intolerant individuals who cannot tolerate milk might still enjoy small portions of aged cheese without issue. This distinction underscores the importance of informed choices rather than blanket avoidance of dairy. By focusing on lactose content and individual tolerance, cheese can remain a part of a balanced diet for many.
Finally, a descriptive approach to managing cheese-related constipation involves mindful consumption and symptom tracking. Keep a food diary to identify specific cheeses and portions that trigger discomfort. Experiment with different types and quantities to determine your personal threshold. For example, some individuals may tolerate up to 1 ounce of high-lactose cheese daily, while others may need to stick to trace-lactose options. Combining cheese with non-dairy, fiber-rich foods can also mitigate its constipating effects. Over time, this awareness allows for a tailored approach to enjoying cheese without sacrificing digestive health.
Does Cheese Contain Fluoride? Uncovering the Truth About Dairy and Fluoride
You may want to see also

Hard vs. Soft Cheeses: Harder cheeses have less lactose, reducing constipation risk compared to softer types
Hard cheeses, such as cheddar or Parmesan, contain significantly less lactose than their softer counterparts like Brie or Camembert. This is because the aging process breaks down much of the lactose, making harder cheeses a better option for those concerned about constipation. Lactose, a sugar found in milk, can be difficult for some people to digest, leading to digestive discomfort, including constipation. By choosing harder cheeses, you can enjoy dairy without the same risk of lactose-related issues.
Consider this scenario: a person with mild lactose intolerance wants to include cheese in their diet but worries about constipation. Opting for harder cheeses allows them to consume dairy with less lactose, potentially reducing digestive problems. For instance, 1 ounce of cheddar contains about 0.03 grams of lactose, whereas the same amount of cream cheese has around 0.6 grams. This difference highlights why harder cheeses are a smarter choice for lactose-sensitive individuals. Pairing these cheeses with high-fiber foods, like whole-grain crackers or vegetables, can further support healthy digestion.
From a practical standpoint, understanding the lactose content in cheeses can help you make informed dietary choices. If you’re prone to constipation, limit softer cheeses and prioritize harder varieties. For example, Swiss cheese (0.1 grams of lactose per ounce) or provolone (0.1 grams per ounce) are excellent alternatives to high-lactose options like cottage cheese (1.6 grams per half-cup). Additionally, portion control matters—even low-lactose cheeses can contribute to constipation if consumed in excess. Stick to recommended serving sizes, typically 1–2 ounces per snack or meal.
A comparative analysis reveals that the texture of cheese directly correlates with its lactose content. Harder cheeses undergo longer aging, which reduces moisture and lactose, while softer cheeses retain more of these elements. This makes softer cheeses creamier but riskier for constipation-prone individuals. For instance, blue cheese, despite being semi-soft, has low lactose due to its aging process, proving that texture isn’t the only factor. However, as a general rule, harder cheeses are a safer bet for minimizing lactose intake and associated digestive issues.
Finally, incorporating harder cheeses into your diet doesn’t mean sacrificing flavor or variety. Experiment with options like aged gouda, pecorino, or Gruyère to find what suits your taste. For those who enjoy softer cheeses, moderation is key—enjoy small portions occasionally rather than daily. Combining harder cheeses with probiotics, such as yogurt or kefir, can also promote gut health and reduce constipation risk. By balancing your cheese choices and being mindful of lactose content, you can savor dairy without compromising digestive comfort.
Mastering the Art of Cheese Tasting: The Professional Aficionado's Title
You may want to see also

Fat Content Impact: High-fat cheeses can slow digestion, potentially leading to constipation in some people
High-fat cheeses, such as cheddar, Parmesan, and cream cheese, can significantly slow digestion due to their dense lipid content. Fats require more time to break down in the stomach, delaying the movement of food through the digestive tract. This sluggish transit time increases the absorption of water from stool, making it harder and more difficult to pass. For individuals prone to constipation, consuming these cheeses in excess can exacerbate the issue. Monitoring portion sizes—limiting intake to 1–2 ounces per serving—can help mitigate this effect while still allowing enjoyment of these rich flavors.
Consider the digestive process as a conveyor belt: high-fat foods act like a bottleneck, slowing everything down. Unlike low-fat options like fresh mozzarella or cottage cheese, which pass through more quickly, high-fat cheeses linger longer in the system. This prolonged stay can be particularly problematic for older adults or those with pre-existing gastrointestinal conditions, whose digestive systems may already operate at a reduced pace. Pairing these cheeses with high-fiber foods, such as whole-grain crackers or raw vegetables, can counteract their constipating effects by promoting regular bowel movements.
From a practical standpoint, moderation is key when incorporating high-fat cheeses into your diet. For example, swapping a 2-ounce serving of cheddar (containing ~12g of fat) for the same amount of part-skim ricotta (containing ~4g of fat) can reduce the digestive burden without sacrificing taste. Additionally, staying hydrated is crucial, as water helps soften stool and aids in its passage. Aim for at least 8–10 cups of fluid daily, especially when consuming high-fat dairy products. For those with persistent issues, consulting a dietitian to tailor cheese choices to individual tolerance levels can be beneficial.
Comparatively, the impact of high-fat cheeses on digestion varies widely among individuals. While some may experience constipation after a single indulgent meal, others might tolerate them without issue. Factors like overall diet, hydration levels, and physical activity play a role in how the body processes these foods. For instance, someone who regularly exercises may have a faster metabolism, reducing the likelihood of constipation from occasional high-fat cheese consumption. Tracking symptoms after meals can help identify personal thresholds and inform dietary adjustments.
Instructively, if you suspect high-fat cheeses are contributing to constipation, start by keeping a food diary to pinpoint patterns. Note portion sizes, types of cheese consumed, and any accompanying symptoms. Gradually reduce intake of high-fat varieties while increasing low-fat alternatives, such as Swiss or feta, which have lower lipid content. Incorporating probiotics, like those found in yogurt or kefir, can also support gut health and improve digestion. Small, mindful changes can lead to significant relief without requiring the elimination of cheese altogether.
Does American Cheese Contain Aluminum? Uncovering the Truth Behind the Myth
You may want to see also
Explore related products
$13.87 $18.49
$9.77 $21.99

Fiber Pairing Tips: Eating cheese with fiber-rich foods can help prevent constipation and improve digestion
Cheese, a beloved staple in many diets, often gets a bad rap for its potential to cause constipation. However, pairing cheese with fiber-rich foods can transform it from a digestive culprit into a balanced component of a gut-friendly meal. Fiber acts as a natural regulator, promoting bowel movements and preventing the sluggishness that can sometimes accompany dairy consumption. By strategically combining cheese with high-fiber options, you can enjoy its creamy texture and rich flavor without the discomfort.
Consider this practical approach: for every ounce of cheese (about 28 grams), aim to pair it with at least 2–3 grams of dietary fiber. For instance, a slice of cheddar (1 ounce) contains around 0.4 grams of fiber, so pairing it with a small apple (4.4 grams of fiber) or a cup of cooked broccoli (5.1 grams) can create a harmonious digestive balance. This ratio ensures that the fiber content outweighs the constipating potential of cheese, keeping your gut moving efficiently.
The science behind this pairing lies in how fiber interacts with the digestive system. Soluble fiber, found in oats, beans, and fruits, absorbs water and softens stool, while insoluble fiber, abundant in vegetables and whole grains, adds bulk. Cheese, being low in fiber and sometimes dehydrating due to its sodium content, can slow digestion. However, when paired with fiber, the moisture retention and bulk provided by fiber counteract these effects, promoting regularity.
For those with sensitive digestive systems or older adults, who are more prone to constipation, this strategy is particularly beneficial. Start by incorporating small portions of cheese into meals already rich in fiber, such as a quinoa salad with feta or a whole-grain cracker topped with goat cheese and sliced pears. Gradually experiment with different combinations to find what works best for your body. Remember, moderation is key—excessive cheese consumption, even with fiber, can still lead to digestive issues.
Incorporating this fiber-pairing technique doesn’t mean sacrificing flavor or creativity. For example, a snack of sharp cheddar with a handful of almonds (3.5 grams of fiber per ounce) or a grilled vegetable sandwich with provolone and spinach (2.2 grams of fiber per cup) can be both satisfying and digestive-friendly. By mindful pairing, cheese can become part of a diet that supports, rather than hinders, digestive health.
Are Cheese Hot Pockets Halal? Exploring Ingredients and Certification
You may want to see also

Individual Sensitivity: Cheese affects everyone differently; monitor your body’s response to identify personal triggers
Cheese, a beloved staple in many diets, doesn’t treat everyone the same. While some can indulge in a creamy brie or sharp cheddar without issue, others may experience discomfort, bloating, or constipation shortly after consumption. This disparity isn’t random—it’s rooted in individual sensitivity, influenced by factors like lactose intolerance, fat content tolerance, and overall digestive health. Understanding your body’s unique response to cheese is the first step in managing its effects.
To pinpoint your personal triggers, adopt a systematic approach. Start by tracking your cheese intake in a food diary, noting the type, quantity, and timing of consumption. Pair this with detailed observations of any digestive symptoms that follow. For instance, hard cheeses like Parmesan contain less lactose than soft cheeses like mozzarella, so comparing reactions to different varieties can reveal lactose as a culprit. Similarly, high-fat cheeses might slow digestion in some individuals, leading to constipation. Over time, patterns will emerge, allowing you to identify specific cheeses or amounts that your body tolerates best.
Age and lifestyle play a role in how cheese affects digestion. Younger adults with robust digestive enzymes may process cheese more efficiently, while older adults might experience increased sensitivity due to natural enzyme decline. Athletes or highly active individuals may metabolize fats differently, reducing the likelihood of constipation from high-fat cheeses. Tailoring your cheese choices to your age, activity level, and overall health can minimize discomfort. For example, older individuals might opt for lactose-free or lower-fat options, while younger, active people could experiment with a wider range of cheeses in moderation.
Practical tips can further help manage cheese-related constipation. Pairing cheese with fiber-rich foods like whole-grain crackers or vegetables can aid digestion and prevent blockages. Staying hydrated is crucial, as water softens stool and promotes regular bowel movements. If you suspect lactose intolerance, try lactose-free cheese alternatives or take lactase enzymes before consuming dairy. Portion control is equally important—limiting servings to 1–2 ounces at a time can reduce the risk of overload. By combining these strategies with personalized observations, you can enjoy cheese without the unwanted side effects.
Ultimately, cheese’s impact on digestion is a highly individual matter. What constipates one person might be harmless to another, making self-monitoring essential. Armed with awareness, experimentation, and practical adjustments, you can navigate your cheese consumption with confidence. Remember, the goal isn’t to eliminate cheese entirely but to find the balance that works for your body. After all, life’s too short to miss out on the joys of cheese—just make sure it’s on your terms.
Are Cheese Hot Pockets Vegetarian? Unraveling the Ingredients and Facts
You may want to see also
Frequently asked questions
Cheese can contribute to constipation in some people due to its low fiber content and high fat, which may slow digestion.
Cheese is low in fiber and can be difficult to digest for some individuals, leading to slower bowel movements and constipation.
Harder, aged cheeses like cheddar are more likely to cause constipation due to their lower moisture content, while softer cheeses like mozzarella may have less impact.
Yes, lactose intolerance can cause digestive issues, including constipation, as the body struggles to break down lactose in cheese.
Pair cheese with high-fiber foods like fruits, vegetables, or whole grains, stay hydrated, and consume cheese in moderation to reduce the risk of constipation.