Cheese, a beloved dairy product enjoyed worldwide, often sparks curiosity about its effects on digestion, particularly in relation to stomach aches. While some individuals claim that cheese can alleviate discomfort, others argue it might exacerbate symptoms due to its lactose content or high fat levels. This raises the question: does cheese genuinely help soothe stomach aches, or could it potentially worsen them? Understanding the relationship between cheese consumption and digestive health requires examining factors such as lactose intolerance, fat content, and individual sensitivities, as well as considering the type of cheese and portion size.
| Characteristics | Values |
|---|---|
| General Effect on Stomach Aches | Cheese can have mixed effects; it may help some individuals but worsen symptoms in others, depending on the type of stomach ache and individual tolerance. |
| Lactose Content | High-lactose cheeses (e.g., fresh cheeses like ricotta) can aggravate stomach aches in lactose-intolerant individuals. |
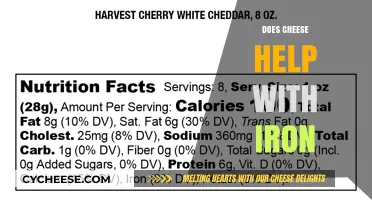
| Low-Lactose Options | Hard cheeses (e.g., cheddar, Swiss) are lower in lactose and may be better tolerated. |
| Fat Content | High-fat cheeses can slow digestion and potentially ease stomach discomfort for some, but may worsen symptoms in those with conditions like gastritis or GERD. |
| Probiotic Properties | Fermented cheeses (e.g., Gouda, cheddar) contain probiotics that may aid digestion and reduce stomach aches in some individuals. |
| Histamine Content | Aged cheeses are high in histamines, which can trigger stomach aches in histamine-intolerant individuals. |
| Individual Tolerance | Effects vary widely; some people find cheese soothing, while others experience bloating, gas, or pain. |
| Recommended for Specific Conditions | Cheese may help with mild indigestion or hunger-related stomach aches but is not advised for conditions like lactose intolerance, IBS, or acid reflux. |
| Portion Size | Small portions are less likely to cause discomfort compared to large servings. |
| Timing of Consumption | Eating cheese with other foods can reduce the risk of stomach aches compared to consuming it on an empty stomach. |
Explore related products
What You'll Learn

Cheese's Probiotic Content and Gut Health
Cheese, a fermented food, often contains live bacteria that can influence gut health. Unlike yogurt, which is widely recognized for its probiotic benefits, cheese’s probiotic content varies significantly by type and production method. Hard cheeses like cheddar or Swiss undergo aging processes that reduce moisture, limiting the survival of live cultures. In contrast, softer, less aged cheeses such as Gouda, mozzarella, and some artisanal varieties retain more live bacteria, including strains like *Lactobacillus* and *Bifidobacterium*. These microorganisms can contribute to a balanced gut microbiome, potentially alleviating stomach discomfort by aiding digestion and reducing inflammation.
To harness cheese’s probiotic potential, focus on raw, unpasteurized, or traditionally fermented varieties. Pasteurization kills beneficial bacteria, so opt for labels indicating "raw milk" or "live cultures." Pairing cheese with prebiotic-rich foods like garlic, onions, or whole grains can enhance its gut-health benefits. For instance, a slice of Gouda on a whole-grain cracker provides both probiotics and fiber, fostering a symbiotic environment for gut flora. However, moderation is key—excessive consumption can lead to lactose intolerance symptoms or calorie overload, counteracting potential benefits.
Not all cheeses are created equal in their gut-health impact. Blue cheese, for example, contains *Penicillium* molds that may offer antimicrobial benefits but lack significant probiotic strains. Similarly, processed cheese products often contain additives and lack live cultures altogether. For targeted gut support, consider cheeses like kefir cheese or cottage cheese, which are made from fermented milk and retain higher levels of live bacteria. Incorporating 1–2 ounces daily as part of a balanced diet can be a practical way to introduce probiotics without relying on supplements.
Age groups and health conditions influence how cheese affects gut health. Children and older adults, whose gut microbiomes may be more sensitive, can benefit from small servings of mild, probiotic-rich cheeses like mild cheddar or fresh cheese curds. Individuals with irritable bowel syndrome (IBS) or lactose intolerance should experiment cautiously, starting with lactose-reduced options like aged Parmesan or lactose-free cheese. Consulting a dietitian can help tailor cheese choices to specific gut health needs, ensuring both safety and efficacy.
Incorporating probiotic-rich cheese into your diet requires awareness of potential drawbacks. While beneficial bacteria can soothe stomach aches by improving digestion, overconsumption or sensitivity to dairy proteins may exacerbate issues like bloating or gas. Pairing cheese with digestive enzymes or consuming it in fermented forms like cheese spreads or whey-based products can minimize these risks. Ultimately, cheese’s role in gut health is nuanced—it’s not a cure-all but a valuable addition to a diverse, fiber-rich diet that supports microbial balance and digestive comfort.
Creative Ways to Repurpose Leftover Lasagna Cheese Filling
You may want to see also

Lactose Intolerance and Stomach Discomfort
Lactose intolerance occurs when the body lacks sufficient lactase, the enzyme needed to break down lactose, a sugar found in milk and dairy products. Without adequate lactase, undigested lactose ferments in the gut, leading to symptoms like bloating, gas, abdominal pain, and diarrhea. While cheese is a dairy product, its lactose content varies widely depending on the type and aging process. Hard cheeses like cheddar or Parmesan contain minimal lactose, often less than 1 gram per ounce, making them better tolerated by many lactose-intolerant individuals. In contrast, soft or fresh cheeses like ricotta or cream cheese retain higher lactose levels, typically 3–5 grams per serving, and are more likely to trigger discomfort.
To manage lactose intolerance effectively, start by identifying your personal tolerance threshold. Gradually introduce small portions of low-lactose cheeses, such as Swiss or gouda, and monitor your body’s response. Pairing cheese with other foods can slow digestion, reducing the likelihood of symptoms. For example, a slice of cheddar on whole-grain bread or a sprinkle of feta on a salad may be better tolerated than cheese consumed alone. Over-the-counter lactase enzymes, taken before eating dairy, can also help break down lactose, potentially allowing for greater cheese consumption without discomfort.
Children and adolescents are less likely to experience lactose intolerance, as lactase production typically declines with age. However, for older adults or those with diagnosed intolerance, experimenting with fermented dairy products like aged cheeses or lactose-free varieties can be a practical solution. Fermentation reduces lactose content naturally, making these options gentler on the stomach. For instance, a 30-gram serving of aged cheddar contains less than 0.5 grams of lactose, compared to 3 grams in the same amount of cottage cheese.
While cheese can sometimes alleviate stomach aches for those without lactose intolerance—thanks to its protein and fat content, which can soothe hunger-related discomfort—it’s a double-edged sword for intolerant individuals. Misjudging lactose content or portion size can exacerbate symptoms rather than relieve them. Keep a food diary to track which cheeses and serving sizes work best for you. For severe intolerance, consider calcium-fortified non-dairy alternatives to meet nutritional needs without risking discomfort. Understanding your body’s limits and making informed choices ensures cheese remains a pleasurable, not painful, part of your diet.
Are White Spots on Cheese Normal? A Complete Guide
You may want to see also

Anti-Inflammatory Properties of Certain Cheeses
Cheese, often maligned for its fat content, harbors surprising anti-inflammatory properties in certain varieties. Fermented cheeses like cheddar, Gouda, and Swiss contain bioactive peptides that inhibit inflammation pathways in the gut. These peptides, formed during the aging process, act as natural modulators of the immune response, potentially soothing stomach aches linked to inflammation. Studies suggest that moderate consumption—around 30-50 grams daily—may provide these benefits without exacerbating digestive issues.
Not all cheeses are created equal in this regard. Soft, fresh cheeses like mozzarella or cream cheese lack the fermentation time needed to produce anti-inflammatory peptides. Opt for aged, hard cheeses with higher protein content, as these are more likely to contain beneficial compounds. Pairing cheese with fiber-rich foods like whole-grain crackers or vegetables can further support gut health by promoting a balanced microbiome, which is crucial for reducing inflammation.
For individuals with lactose intolerance, the anti-inflammatory benefits of cheese may be overshadowed by digestive discomfort. However, aged cheeses naturally contain lower lactose levels due to fermentation. Hard cheeses like Parmesan or aged cheddar typically contain less than 1 gram of lactose per ounce, making them a safer option. Start with small portions to gauge tolerance and gradually increase intake if no adverse effects occur.
Incorporating anti-inflammatory cheeses into your diet requires mindful selection and portion control. Avoid processed cheese products, which often contain additives that negate health benefits. Instead, choose organic, grass-fed varieties, as they tend to have higher levels of conjugated linoleic acid (CLA), another compound with anti-inflammatory properties. For optimal results, combine cheese consumption with other anti-inflammatory foods like turmeric, ginger, or leafy greens to amplify its effects.
While cheese alone isn’t a cure-all for stomach aches, its anti-inflammatory properties make it a valuable addition to a gut-friendly diet. Focus on aged, fermented varieties, monitor portion sizes, and pair with complementary foods to maximize benefits. As always, consult a healthcare provider if stomach aches persist, as underlying conditions may require targeted treatment.
Aged Cheeses and Lactose: What You Need to Know
You may want to see also
Explore related products

Impact of Fermented Cheese on Digestion
Fermented cheese, such as cheddar, Gouda, and Swiss, contains probiotics—beneficial bacteria that support gut health. These microorganisms can aid digestion by breaking down lactose and other complex compounds, potentially alleviating stomach discomfort for some individuals. However, the impact varies depending on the type of cheese, its fermentation process, and the person’s digestive tolerance. For instance, aged cheeses like Parmesan have lower lactose content, making them easier to digest for those with mild lactose intolerance.
To harness the digestive benefits of fermented cheese, start with small portions—around 1–2 ounces (30–60 grams) per serving. Pair it with fiber-rich foods like whole-grain crackers or fresh fruit to promote balanced digestion. Avoid overeating, as excessive cheese consumption can lead to bloating or constipation due to its high fat content. For children or older adults, opt for milder, softer cheeses like mozzarella or young cheddar, which are gentler on the stomach.
A comparative analysis reveals that fermented cheese outperforms fresh cheese in aiding digestion. Fresh cheeses like ricotta or cottage cheese lack the probiotic benefits of fermented varieties, making them less effective for stomach aches. Fermented cheeses also contain enzymes like lipase, which assist in fat digestion, reducing the likelihood of discomfort after meals. However, individuals with severe lactose intolerance or dairy allergies should still exercise caution, as even fermented cheese may trigger symptoms.
Practically, incorporating fermented cheese into your diet requires mindful selection. Choose raw milk cheeses, as pasteurization can destroy beneficial bacteria. Look for labels indicating "live and active cultures" to ensure probiotic content. For those with persistent stomach issues, consult a dietitian to determine if fermented cheese is a suitable addition to your diet. While it may not be a cure-all, fermented cheese can be a flavorful, functional food to support digestive health when consumed thoughtfully.
Discover Glendale's Best Cheesecake Spots: A Sweet Guide
You may want to see also

Cheese Fat Content and Stomach Irritation
Cheese, a beloved dairy product, varies widely in fat content, which can significantly impact its effects on stomach irritation. High-fat cheeses, such as cheddar or gouda, contain upwards of 30% fat, while low-fat options like part-skim mozzarella hover around 15%. This fat content influences digestion speed and potential discomfort. High-fat cheeses slow gastric emptying, which can exacerbate feelings of fullness or bloating in sensitive individuals. Conversely, low-fat cheeses may be gentler on the stomach, making them a better choice for those prone to irritation.
Consider the role of fat in triggering acid reflux, a common cause of stomach aches. Fatty foods relax the lower esophageal sphincter, allowing stomach acid to flow back into the esophagus. For individuals with gastroesophageal reflux disease (GERD), even moderate portions of high-fat cheese can worsen symptoms. A practical tip: limit high-fat cheese intake to small servings (e.g., 1 oz) and pair it with fiber-rich foods like whole-grain crackers to mitigate its effects.
Not all fats are created equal, and the type of fat in cheese matters. Hard cheeses like parmesan contain saturated fats, which are more likely to irritate the stomach lining compared to softer cheeses with higher unsaturated fat content, such as goat cheese. For those with lactose intolerance, fat content can compound issues, as high-fat cheeses slow digestion, prolonging exposure to lactose. Opting for lactose-free or low-fat varieties may alleviate discomfort.
Age and metabolism also play a role in how cheese fat affects the stomach. Younger individuals with robust digestive systems may tolerate high-fat cheeses better than older adults, whose digestive efficiency declines. For seniors or those with sluggish digestion, low-fat or fermented cheeses like feta or cottage cheese are advisable. A comparative approach: while high-fat cheeses offer rich flavor, their impact on stomach irritation often outweighs the sensory benefits for sensitive groups.
In summary, cheese fat content is a critical factor in its potential to soothe or irritate the stomach. Low-fat, lactose-free, or fermented options are generally safer for those prone to discomfort. Portion control and mindful pairing with other foods can further reduce irritation. By understanding these nuances, individuals can enjoy cheese without compromising digestive health.
Perfect Side Dish Ideas for Bean and Cheese Burritos
You may want to see also
Frequently asked questions
Cheese is not typically recommended for stomach aches, as it can be hard to digest and may worsen symptoms, especially in those with lactose intolerance.
Eating cheese is unlikely to soothe an upset stomach, as it is high in fat and can slow digestion, potentially aggravating discomfort.
Cheese is generally not good for stomach pain caused by indigestion, as its high fat content can delay stomach emptying and increase discomfort.
Cheese is not advisable for stomach aches from diarrhea, as dairy products can sometimes exacerbate gastrointestinal symptoms, especially in sensitive individuals.
Small amounts of mild, low-fat cheese might be tolerated by some, but it’s not a proven remedy for stomach aches and may not provide relief for everyone.