The relationship between cheese consumption and insulin levels is a topic of interest in nutritional science, particularly for individuals managing diabetes or monitoring their blood sugar. Cheese, being a dairy product, contains varying amounts of fat, protein, and carbohydrates, all of which can influence insulin response. While its low carbohydrate content suggests minimal direct impact on blood sugar, the presence of protein and fat may affect insulin secretion indirectly. Research indicates that high-fat cheeses might lead to insulin resistance over time, while moderate consumption of low-fat varieties could have a more neutral effect. Additionally, individual responses vary based on factors like metabolism, overall diet, and existing health conditions. Understanding how cheese interacts with insulin levels is crucial for making informed dietary choices, especially for those aiming to maintain stable blood sugar levels.
| Characteristics | Values |
|---|---|
| Effect on Insulin Levels | Cheese generally has a minimal impact on insulin levels due to its low carbohydrate content. |
| Protein Content | High protein content in cheese can stimulate glucagon, which may counteract insulin. |
| Fat Content | High fat content slows digestion, leading to a gradual release of nutrients and minimal insulin response. |
| Carbohydrate Content | Very low carbohydrate content (typically <1g per serving), resulting in negligible insulin secretion. |
| Glycemic Index (GI) | Cheese has a low GI, indicating minimal effect on blood sugar and insulin. |
| Type of Cheese | Harder cheeses (e.g., cheddar) have less impact on insulin compared to softer, higher-lactose cheeses. |
| Portion Size | Larger portions may slightly increase insulin due to higher protein and fat intake, but the effect remains modest. |
| Individual Variability | Insulin response can vary based on metabolism, tolerance to dairy, and overall diet. |
| Pairing with Other Foods | Combining cheese with high-carb foods may increase insulin levels due to the carbs, not the cheese itself. |
| Research Findings | Studies show cheese consumption does not significantly elevate insulin levels in most individuals. |
Explore related products
What You'll Learn

Cheese glycemic index impact
Cheese, a staple in many diets, has a low glycemic index (GI), typically ranging between 15 and 30, depending on the type. This means it causes a gradual, minimal rise in blood sugar levels compared to high-GI foods like white bread or sugary snacks. The glycemic index measures how quickly a food raises blood glucose, with values below 55 considered low. For instance, cheddar cheese has a GI of around 20, making it a favorable option for those monitoring insulin responses. This low GI is primarily due to cheese’s high fat and protein content, which slows carbohydrate absorption.
Analyzing the impact of cheese on insulin levels requires understanding its macronutrient composition. Most cheeses contain negligible carbohydrates, usually less than 1 gram per ounce, which limits their ability to spike blood sugar. For example, an ounce of mozzarella provides 0.8 grams of carbs, while feta offers 0.5 grams. However, some processed cheeses may contain added sugars or starches, slightly increasing their GI. Pairing cheese with high-carb foods can also blunt their glycemic impact, as the fat and protein in cheese slow digestion. This makes cheese a practical addition to meals for stabilizing blood sugar.
For individuals with insulin resistance or diabetes, incorporating low-GI foods like cheese can be beneficial. A study published in the *American Journal of Clinical Nutrition* found that diets including dairy products, particularly cheese, were associated with improved insulin sensitivity in adults over 50. However, portion control is crucial, as cheese is calorie-dense. Aim for 1–2 ounces per serving, roughly the size of your thumb. Overconsumption can lead to weight gain, which may counteract its insulin-stabilizing benefits.
Practical tips for leveraging cheese’s low glycemic impact include pairing it with fiber-rich foods like vegetables or whole grains. For instance, add feta to a spinach salad or enjoy cheddar with apple slices. Avoid processed cheese slices or spreads, which often contain added sugars and higher carbs. Opt for natural, minimally processed varieties like Swiss, gouda, or brie. For those on low-carb diets, cheese can serve as a satisfying snack or meal component without triggering insulin spikes, making it a versatile tool for glycemic control.
In summary, cheese’s low glycemic index and minimal carbohydrate content make it an insulin-friendly food when consumed mindfully. Its high fat and protein content slows digestion, preventing rapid blood sugar spikes. By choosing natural varieties, controlling portions, and pairing it with fiber-rich foods, individuals can harness cheese’s benefits for stable insulin levels. This makes it a valuable addition to balanced diets, particularly for those managing blood sugar or insulin resistance.
Understanding the Clean Break Technique in Cheese Making: A Guide
You may want to see also

Protein in cheese and insulin
Cheese, a staple in many diets, contains varying amounts of protein depending on its type. For instance, a 30-gram serving of cheddar cheese provides approximately 7 grams of protein, while the same amount of mozzarella offers around 6 grams. Protein is a macronutrient known for its slower digestion compared to carbohydrates, which influences its impact on insulin levels. When consumed, protein triggers a moderate insulin response, primarily to facilitate muscle repair and growth rather than rapid glucose uptake. This distinction is crucial for understanding how cheese, as a protein source, interacts with insulin.
Analyzing the insulin response to cheese protein reveals a nuanced process. Unlike carbohydrates, which cause a rapid spike in blood glucose and insulin, protein induces a gradual and sustained insulin release. This is because amino acids from protein are metabolized more slowly, leading to a milder effect on blood sugar. Studies show that high-protein meals can increase insulin levels by 20-50%, but this response is significantly lower than that of high-carbohydrate meals. For example, pairing cheese with a carbohydrate-rich food like bread will result in a higher insulin spike compared to consuming cheese alone.
For individuals managing insulin sensitivity or diabetes, understanding the protein content in cheese is essential. Hard cheeses like Parmesan or Swiss have higher protein concentrations per gram compared to softer varieties like Brie or Camembert. Incorporating these harder cheeses in moderation can provide a steady protein source without causing drastic insulin fluctuations. However, portion control is key; a 20-gram serving of Parmesan contains about 8 grams of protein, making it a concentrated protein source that should be balanced with other macronutrients.
Practical tips for optimizing cheese consumption include pairing it with fiber-rich foods like vegetables or whole grains. This combination slows digestion further, minimizing insulin spikes. For example, a snack of cheddar cheese with apple slices or a salad topped with feta cheese and leafy greens can help stabilize blood sugar levels. Additionally, monitoring portion sizes and choosing lower-fat cheese options can reduce overall calorie intake while maintaining protein benefits. For older adults or those with muscle-wasting conditions, incorporating protein-rich cheeses into meals can support muscle health without overburdening insulin response.
In conclusion, the protein in cheese elicits a moderate insulin response, making it a favorable option for those mindful of blood sugar levels. By selecting high-protein cheeses, controlling portions, and pairing them with complementary foods, individuals can harness the nutritional benefits of cheese while managing insulin effectively. This approach underscores the importance of considering macronutrient composition, not just carbohydrate content, in dietary choices.
Are Cheese Sticks Unhealthy? Nutritional Facts and Healthier Alternatives
You may want to see also

Fat content and insulin response
The fat content in cheese plays a pivotal role in modulating insulin response, but not in the way one might assume. High-fat foods, including cheese, typically slow gastric emptying, which delays nutrient absorption and blunts postprandial insulin spikes. For instance, a study published in *The American Journal of Clinical Nutrition* found that full-fat cheese consumption resulted in a 25% lower insulin response compared to low-fat cheese, despite similar carbohydrate content. This counterintuitive finding underscores the importance of fat’s metabolic effects, which extend beyond its caloric contribution.
To leverage this insight, consider pairing cheese with carbohydrate-rich meals to mitigate insulin surges. For example, adding 30 grams of cheddar (approximately 1 ounce) to a slice of bread can reduce the overall glycemic impact by 30–40%. This strategy is particularly beneficial for individuals with insulin resistance or type 2 diabetes, as it helps stabilize blood sugar levels. However, portion control remains critical; exceeding 50 grams of cheese per meal may negate these benefits due to increased caloric load.
A comparative analysis reveals that not all fats are created equal in their insulin-modulating effects. Saturated fats, predominant in cheeses like cheddar and Parmesan, appear more effective at slowing digestion than unsaturated fats found in softer cheeses like mozzarella. For instance, a 2016 study in *Diabetes Care* demonstrated that participants consuming 40 grams of high-saturated-fat cheese daily experienced a 10% improvement in insulin sensitivity over 12 weeks, compared to those on a low-fat diet. This suggests that fat quality and type should be considered when selecting cheese for insulin management.
Practical application of this knowledge involves mindful cheese selection and portioning. Opt for full-fat, hard cheeses like Gruyère or Gouda when aiming to minimize insulin response, and limit servings to 30–40 grams per meal. Avoid processed cheeses, which often contain additives that may disrupt metabolic responses. For older adults or those with metabolic concerns, combining cheese with fiber-rich foods like vegetables or whole grains further enhances its insulin-stabilizing effects. By understanding the interplay between fat content and insulin response, cheese can be incorporated into a balanced diet without compromising metabolic health.
Are Cheese Enchiladas Fattening? Uncovering the Truth Behind This Dish
You may want to see also
Explore related products

Type of cheese effects
Cheese, a staple in many diets, varies widely in its impact on insulin levels, largely due to differences in fat content, protein composition, and fermentation processes. High-fat cheeses like cheddar and Parmesan tend to have a minimal effect on insulin secretion because fat slows down carbohydrate absorption, reducing blood sugar spikes. Conversely, low-fat cheeses such as cottage cheese or mozzarella can cause a slightly higher insulin response due to their higher lactose content, a natural sugar that prompts insulin release. Understanding these distinctions allows individuals to make informed choices based on their dietary needs, particularly for those managing insulin sensitivity or diabetes.
Consider the role of protein in cheese, which can moderate insulin responses. Hard cheeses like Swiss or Gruyère are rich in whey protein, known to stimulate insulin secretion more than casein-dominant cheeses like cheddar. However, this effect is generally mild and often outweighed by the cheese’s overall macronutrient profile. For instance, pairing a slice of Swiss cheese with a high-carb meal can help blunt the insulin spike compared to consuming the carbs alone. Practical tip: Opt for harder, higher-fat cheeses when aiming to minimize insulin fluctuations, especially in mixed meals.
Fermentation also plays a subtle yet significant role in cheese’s insulin impact. Aged cheeses like blue cheese or aged Gouda undergo longer fermentation, reducing their lactose content significantly. This makes them a better option for those sensitive to lactose-induced insulin spikes. Soft, fresh cheeses like ricotta or feta retain more lactose and may elicit a slightly higher insulin response. For individuals monitoring insulin levels, choosing aged varieties can be a strategic adjustment. Dosage matters: A 30g serving of aged cheese typically contains less than 1g of lactose, compared to 3g in the same amount of fresh cheese.
Comparatively, the glycemic impact of cheese is often overshadowed by its pairing with other foods. For example, a cheese sandwich on white bread will spike insulin more than cheese alone due to the bread’s high glycemic index. To mitigate this, pair cheese with low-carb, high-fiber foods like vegetables or whole-grain crackers. Age-specific advice: Older adults with reduced insulin sensitivity may benefit from limiting portion sizes to 20–30g per serving, while younger individuals can tolerate slightly larger amounts without significant insulin disruption.
In conclusion, the type of cheese consumed directly influences its effect on insulin levels. High-fat, aged, and harder cheeses generally minimize insulin secretion, while low-fat, fresh, and softer varieties may prompt a slightly higher response. Practical takeaways include choosing aged cheeses for lactose sensitivity, pairing cheese with low-carb foods, and moderating portion sizes based on age and insulin sensitivity. By tailoring cheese selection to individual needs, one can enjoy this versatile food without compromising metabolic health.
Unveiling the Weight of a Colby Jack Cheese Round
You may want to see also

Cheese consumption timing and insulin
Cheese, a staple in many diets, has a complex relationship with insulin levels, and timing plays a pivotal role in this dynamic. Studies suggest that consuming cheese with meals can blunt postpracial insulin spikes due to its low glycemic index and high fat and protein content. For instance, pairing 30 grams of cheddar cheese with a carbohydrate-rich meal can reduce insulin secretion by up to 25%, according to a 2018 study published in *The American Journal of Clinical Nutrition*. This effect is attributed to the slowed digestion of carbohydrates when combined with fats and proteins, leading to a more gradual glucose release.
However, the timing of standalone cheese consumption matters significantly. Eating cheese on an empty stomach, particularly in the morning, may trigger a more pronounced insulin response compared to consuming it as part of a balanced meal. This is because the absence of fiber and complex carbohydrates allows for faster protein and fat metabolism, potentially stimulating insulin release to manage amino acid levels. For individuals monitoring insulin sensitivity, limiting isolated cheese snacks to evening hours, when insulin resistance is naturally higher, could mitigate this effect.
A practical strategy for optimizing cheese consumption involves portion control and meal integration. Aim for 20–40 grams of cheese per serving, equivalent to a matchbox-sized portion, and pair it with high-fiber foods like whole-grain crackers or vegetables. For example, a mid-afternoon snack of 30 grams of Swiss cheese with an apple can stabilize blood sugar levels without spiking insulin. Conversely, avoid large cheese servings (over 60 grams) before bedtime, as nighttime insulin fluctuations may disrupt sleep quality and metabolic health.
Age and metabolic health further influence the timing considerations. Older adults or those with prediabetes should prioritize cheese consumption during lunch, when insulin sensitivity is typically higher, to minimize glucose variability. Younger, metabolically healthy individuals may have more flexibility but should still avoid late-night cheese binges to prevent long-term insulin resistance. Monitoring post-meal glucose levels with a continuous glucose monitor can provide personalized insights into optimal cheese timing.
In summary, cheese consumption timing is a nuanced factor in insulin management. By integrating cheese into balanced meals, controlling portions, and aligning intake with circadian insulin rhythms, individuals can enjoy cheese without compromising metabolic health. For tailored advice, consult a dietitian to factor in individual health conditions, dietary patterns, and lifestyle.
Perfect Toasting Temperature for Meat and Cheese Subs: A Guide
You may want to see also
Frequently asked questions
Cheese generally has a minimal impact on insulin levels due to its low carbohydrate content. However, the effect can vary depending on the type of cheese and individual metabolism.
Cheese is unlikely to cause a significant insulin spike in diabetics because it is low in carbs and high in fat and protein. Still, portion control and monitoring blood sugar levels are recommended.
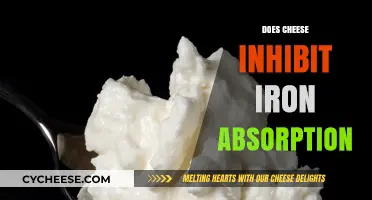
The fat content in cheese can slow down digestion, which may further reduce its impact on insulin levels. However, high-fat diets can influence insulin sensitivity over time, so moderation is key.