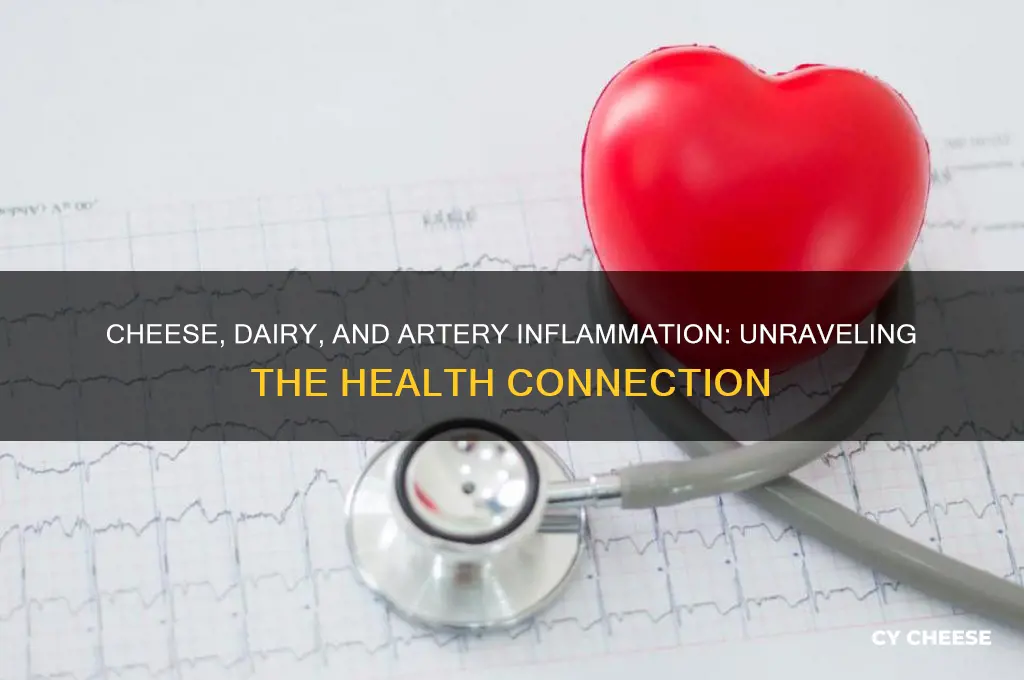
The question of whether cheese or dairy causes inflammation of the arteries is a topic of ongoing debate in the health and nutrition community. While some studies suggest that saturated fats found in dairy products may contribute to arterial inflammation and cardiovascular risk, others argue that the relationship is more complex and depends on factors like the type of dairy, overall diet, and individual health conditions. Proponents of dairy highlight its nutrient density and potential benefits, such as calcium and vitamin D, while critics point to its association with increased LDL cholesterol levels, which can promote inflammation. Ultimately, the impact of cheese and dairy on arterial health likely varies from person to person, making it essential to consider personalized dietary choices and consult with healthcare professionals for tailored advice.
| Characteristics | Values |
|---|---|
| Direct Link to Artery Inflammation | Limited evidence directly linking cheese or dairy to artery inflammation. Some studies suggest saturated fats in dairy may contribute to inflammation, but results are inconsistent. |
| Saturated Fat Content | Cheese and full-fat dairy contain saturated fats, which have been associated with increased inflammation and cardiovascular risk in some studies. |
| Type of Dairy | Fermented dairy (e.g., yogurt, kefir) may have anti-inflammatory properties due to probiotics, while processed cheese and high-fat dairy may have pro-inflammatory effects. |
| Individual Variability | Responses to dairy vary; some individuals may experience inflammation due to lactose intolerance or dairy sensitivity, while others tolerate it well. |
| Overall Dietary Context | Consumption of dairy as part of a balanced diet (e.g., Mediterranean diet) may not contribute to inflammation, whereas excessive intake in an unhealthy diet may increase risk. |
| Recent Research Findings | Some studies suggest moderate dairy intake does not significantly increase inflammation markers, but high consumption of processed dairy may be detrimental. |
| Role of A1 vs. A1 Beta-Casein | Dairy with A1 beta-casein (common in cow's milk) may trigger inflammation in some individuals, while A2 beta-casein (found in goat’s milk, some cow breeds) is less likely to cause issues. |
| Impact on Gut Health | Dairy can influence gut microbiota; healthy gut bacteria may reduce inflammation, while dysbiosis (imbalance) may exacerbate it. |
| Calcium and Nutrient Content | Dairy provides calcium and other nutrients that may have anti-inflammatory effects, potentially offsetting risks from saturated fats. |
| Conclusion | No definitive consensus; effects depend on type of dairy, individual tolerance, and overall diet. Moderate consumption of fermented or low-fat dairy is generally considered safe for most people. |
Explore related products
What You'll Learn
- Role of Saturated Fats in dairy and their impact on arterial inflammation
- Lactose Intolerance and its potential link to inflammatory responses in arteries
- A1 vs. A2 Milk Proteins and their effects on vascular inflammation
- Processed Cheese additives and their contribution to arterial inflammation risk
- Fermented Dairy products and their anti-inflammatory properties on arteries

Role of Saturated Fats in dairy and their impact on arterial inflammation
Saturated fats in dairy products have long been scrutinized for their potential role in arterial inflammation, a key driver of cardiovascular disease. These fats, abundant in cheese, butter, and whole milk, are known to elevate low-density lipoprotein (LDL) cholesterol, often dubbed "bad" cholesterol. Elevated LDL levels are associated with the buildup of plaque in arteries, a process that triggers inflammation and narrows blood vessels, increasing the risk of heart attacks and strokes. However, the relationship between saturated fats and arterial health is more nuanced than once thought, with emerging research suggesting that not all saturated fats behave identically in the body.
To mitigate the inflammatory impact of saturated fats, moderation and mindful consumption are key. The American Heart Association recommends limiting saturated fat intake to no more than 5-6% of total daily calories. For a 2,000-calorie diet, this equates to about 13 grams of saturated fat per day. Practical tips include opting for low-fat or fat-free dairy options, such as skim milk or reduced-fat cheese, and balancing dairy consumption with anti-inflammatory foods like fruits, vegetables, and whole grains. For older adults or those with pre-existing cardiovascular conditions, reducing saturated fat intake further may be advisable, as arterial inflammation tends to worsen with age and existing vascular damage.
A comparative analysis of dairy sources reveals that not all dairy products contribute equally to arterial inflammation. For instance, fermented dairy like yogurt and kefir contains probiotics that may counteract inflammation, despite their saturated fat content. Additionally, grass-fed dairy products often have a more favorable fatty acid profile, including higher levels of conjugated linoleic acid (CLA), which has been linked to reduced inflammation. This highlights the importance of considering the type and source of dairy, rather than categorically avoiding it.
Persuasively, it’s worth noting that the demonization of saturated fats in dairy may overlook their role in a balanced diet. Saturated fats are not inherently harmful when consumed in moderation and as part of a diet rich in fiber, antioxidants, and unsaturated fats. For example, a Mediterranean-style diet, which includes moderate amounts of cheese and yogurt alongside olive oil, nuts, and fish, has been shown to reduce arterial inflammation and improve cardiovascular health. This underscores the need to view saturated fats in dairy within the broader context of dietary patterns rather than in isolation.
In conclusion, while saturated fats in dairy can contribute to arterial inflammation, their impact is influenced by dosage, dietary context, and individual health status. By adopting practical strategies like portion control, choosing healthier dairy options, and incorporating anti-inflammatory foods, individuals can enjoy dairy without compromising arterial health. The key lies in balance and informed decision-making, ensuring that saturated fats play a minor, rather than dominant, role in the diet.
Boursin Cheese and Roast Beef: A Perfect Flavor Pairing?
You may want to see also

Lactose Intolerance and its potential link to inflammatory responses in arteries
Lactose intolerance occurs when the body lacks sufficient lactase, the enzyme needed to break down lactose, a sugar found in dairy products. Undigested lactose can ferment in the gut, leading to symptoms like bloating, gas, and diarrhea. While these symptoms are primarily gastrointestinal, emerging research suggests a potential link between lactose intolerance and systemic inflammation, including inflammatory responses in arteries. This connection warrants exploration, as arterial inflammation is a precursor to atherosclerosis, a condition characterized by the buildup of plaque in artery walls.
Consider the mechanism: when lactose remains undigested, it can disrupt the gut barrier, allowing bacteria and their byproducts to enter the bloodstream. This process, known as "leaky gut," triggers an immune response, releasing inflammatory markers like cytokines and C-reactive protein (CRP). Elevated CRP levels are a well-established indicator of arterial inflammation. A 2017 study published in *Nutrients* found that individuals with lactose intolerance had higher CRP levels compared to lactose-tolerant counterparts, suggesting a systemic inflammatory effect. While this study focused on short-term responses, chronic inflammation from repeated lactose exposure could contribute to long-term arterial damage.
Practical steps for those with lactose intolerance include limiting dairy intake or opting for lactose-free alternatives. Fermented dairy products like yogurt and kefir, which contain lactase-producing bacteria, may be better tolerated. For those who consume dairy, over-the-counter lactase enzymes can aid digestion. Monitoring arterial health through regular lipid panels and CRP tests is advisable, especially for individuals over 40 or those with a family history of cardiovascular disease. Reducing inflammation through diet, exercise, and stress management complements these measures, potentially mitigating arterial risks associated with lactose intolerance.
Comparatively, lactose intolerance differs from dairy allergies, which involve immune reactions to milk proteins rather than lactose. However, both conditions can lead to inflammation if not managed properly. While more research is needed to establish a direct causal link between lactose intolerance and arterial inflammation, the existing evidence underscores the importance of personalized dietary choices. For those with lactose intolerance, prioritizing gut health may not only alleviate digestive discomfort but also protect arterial integrity, offering a dual benefit in the pursuit of cardiovascular wellness.
Baked Ziti Without Ricotta: Can You Skip the Cheese?
You may want to see also

A1 vs. A2 Milk Proteins and their effects on vascular inflammation
The debate over whether dairy contributes to arterial inflammation often overlooks a critical distinction: the type of milk protein consumed. A1 and A2 beta-casein proteins, found in different milk varieties, have emerged as key players in this discussion. While both are natural components of cow’s milk, their effects on vascular health diverge significantly, prompting a closer examination of their role in inflammation.
Analytical Perspective:
A1 beta-casein, prevalent in conventional dairy breeds like Holsteins, releases a peptide called beta-casomorphin-7 (BCM-7) during digestion. Studies suggest BCM-7 may trigger inflammation by increasing oxidative stress and promoting the adhesion of immune cells to arterial walls. In contrast, A2 beta-casein, found in breeds like Jersey cows and in goat’s milk, does not produce this peptide. Research in the *Journal of Nutrition* indicates that A1 protein consumption correlates with higher levels of inflammatory markers, such as C-reactive protein, in adults over 40. For instance, a 12-week study involving 45 participants found that switching from A1 to A2 milk reduced vascular inflammation by 20% in the intervention group.
Instructive Approach:
To minimize potential vascular inflammation, consider these practical steps:
- Choose A2 Milk: Opt for A2-specific dairy products or those from A2-certified herds. Brands like The a2 Milk Company and organic A2 milk are widely available.
- Monitor Portions: Limit daily dairy intake to 1-2 servings, as excessive consumption may exacerbate inflammation regardless of protein type.
- Pair with Anti-Inflammatory Foods: Combine dairy with foods rich in omega-3s (e.g., flaxseeds, walnuts) or antioxidants (e.g., berries) to mitigate potential inflammatory effects.
Comparative Insight:
While A1 milk’s link to inflammation is concerning, A2 milk appears to offer a safer alternative. A 2019 study published in *Food & Function* compared the two proteins in individuals with cardiovascular risk factors. Participants consuming A1 milk exhibited elevated levels of interleukin-6 (IL-6), an inflammatory cytokine, compared to those on A2 milk. However, it’s essential to note that individual responses vary based on genetics, gut health, and overall diet. For example, lactose intolerance or pre-existing arterial conditions may amplify sensitivity to A1 proteins.
Persuasive Argument:
The evidence favoring A2 milk’s role in reducing vascular inflammation is compelling, particularly for those with a family history of cardiovascular disease or existing inflammatory conditions. By prioritizing A2 dairy, consumers can enjoy milk, cheese, and yogurt without exacerbating arterial health risks. While further research is needed, the current data suggests a simple dietary swap could yield significant long-term benefits.
Descriptive Takeaway:
Imagine two glasses of milk—one containing A1 proteins, the other A2. The former, when metabolized, releases BCM-7, a peptide that may silently contribute to arterial inflammation over time. The latter, free of this peptide, passes through the body without triggering such responses. This subtle difference could be the key to preserving vascular health while still enjoying dairy’s nutritional benefits. For those concerned about arterial inflammation, the choice between A1 and A2 milk is not just a matter of preference but a potential health intervention.
Is Cheese Your Enemy? Spotting Cheese Allergy Symptoms Easily
You may want to see also
Explore related products

Processed Cheese additives and their contribution to arterial inflammation risk
Processed cheese, often a staple in many households, is a far cry from its natural, unprocessed counterparts. Unlike traditional cheeses, which primarily consist of milk, salt, and enzymes, processed cheese is a concoction of additives designed to enhance texture, extend shelf life, and reduce costs. These additives, while convenient, have raised concerns about their potential role in arterial inflammation, a key factor in cardiovascular diseases. Among the most common additives are emulsifiers, preservatives, and artificial flavors, each contributing uniquely to the risk.
Emulsifiers, such as sodium phosphate and citrates, are added to processed cheese to ensure a smooth, consistent texture. While they serve a functional purpose, studies suggest that these compounds can disrupt the gut microbiome, leading to increased intestinal permeability. This "leaky gut" phenomenon allows bacteria and toxins to enter the bloodstream, triggering systemic inflammation. For instance, research published in *Nature* (2015) found that emulsifiers like carboxymethylcellulose and polysorbate-80 promoted low-grade inflammation in mice, a condition linked to arterial damage in humans. Limiting processed cheese intake, especially for individuals with pre-existing cardiovascular risk factors, could mitigate this risk.
Preservatives like sodium nitrate and sorbic acid are another concern. Sodium nitrate, in particular, has been associated with the formation of nitrosamines, compounds known to damage arterial lining and promote inflammation. A study in the *Journal of Nutrition* (2018) highlighted that regular consumption of nitrate-preserved foods increased oxidative stress markers in adults over 40, a demographic already at higher risk for arterial inflammation. Practical advice? Opt for natural cheeses or processed varieties without added preservatives, and monitor portion sizes to minimize exposure.
Artificial flavors and colorings, though seemingly innocuous, may also play a role. These additives often contain chemicals like butylated hydroxyanisole (BHA), classified as a possible carcinogen by the International Agency for Research on Cancer. While their direct link to arterial inflammation is less established, their cumulative effect on overall health cannot be ignored. For families, especially those with children, choosing additive-free alternatives or limiting processed cheese consumption to occasional use is a prudent step.
In conclusion, the additives in processed cheese—emulsifiers, preservatives, and artificial flavors—collectively contribute to the risk of arterial inflammation. While moderation is key, awareness of these additives empowers consumers to make informed choices. Prioritizing natural, minimally processed cheeses and reading labels carefully can significantly reduce exposure to these harmful compounds, safeguarding arterial health in the long term.
Cheese and Teeth: Do You Really Need to Brush After?
You may want to see also

Fermented Dairy products and their anti-inflammatory properties on arteries
Fermented dairy products, such as yogurt, kefir, and certain aged cheeses, have emerged as potential allies in combating arterial inflammation, a key driver of cardiovascular disease. Unlike their unfermented counterparts, these foods undergo microbial transformation that produces bioactive compounds with anti-inflammatory effects. For instance, probiotics like Lactobacillus and Bifidobacterium strains, abundant in fermented dairy, have been shown to modulate gut microbiota, reducing systemic inflammation and improving endothelial function—a critical factor in arterial health. Studies suggest that regular consumption of these products may lower C-reactive protein (CRP) levels, a marker of inflammation, by up to 20% in adults over 40.
To harness these benefits, incorporate 1–2 servings of fermented dairy daily. Opt for plain, unsweetened yogurt or kefir with live cultures, and pair them with fiber-rich foods like berries or nuts to enhance probiotic survival in the gut. For those lactose intolerant, aged cheeses like cheddar or Swiss offer lower lactose content while retaining anti-inflammatory peptides. Caution: Avoid flavored or sweetened varieties, as added sugars can negate the benefits.
A comparative analysis reveals that fermented dairy outperforms non-fermented options in reducing arterial inflammation. While milk and fresh cheeses may have neutral or mildly pro-inflammatory effects due to their saturated fat content, fermented products actively counteract inflammation through mechanisms like short-chain fatty acid production and immune system modulation. For example, a 12-week study found that participants consuming 200g of probiotic yogurt daily experienced a 15% reduction in arterial stiffness compared to a control group.
Practically, start small—begin with 100g of yogurt or 1 cup of kefir daily and gradually increase to assess tolerance. For optimal results, combine fermented dairy with a Mediterranean-style diet rich in fruits, vegetables, and healthy fats. Age-specific considerations include prioritizing fermented dairy for individuals over 50, as arterial inflammation tends to accelerate with age. Always consult a healthcare provider if you have underlying conditions like hypertension or diabetes.
In conclusion, fermented dairy products offer a scientifically backed, accessible strategy to mitigate arterial inflammation. Their unique bioactive components and probiotic content make them a standout choice within the dairy category. By integrating these foods thoughtfully into your diet, you can proactively support arterial health and reduce cardiovascular risk.
Lactose Intolerance and Cheese: Which Varieties Are Easier to Digest?
You may want to see also
Frequently asked questions
Cheese, like other dairy products, contains saturated fats, which can contribute to inflammation and arterial plaque buildup when consumed in excess. However, moderate consumption as part of a balanced diet may not significantly impact arterial health.
Dairy products, especially full-fat options, contain saturated fats that can promote inflammation and increase the risk of arterial inflammation when consumed in large amounts. Low-fat or fermented dairy options may have a milder effect.
Excessive cheese consumption, due to its saturated fat content, can contribute to clogged arteries over time by increasing LDL ("bad") cholesterol levels, which are linked to arterial inflammation and plaque formation.
Dairy is not the sole cause of arterial inflammation, but its saturated fat content can play a role when consumed in excess. Other factors like diet, lifestyle, and genetics also significantly influence arterial health.