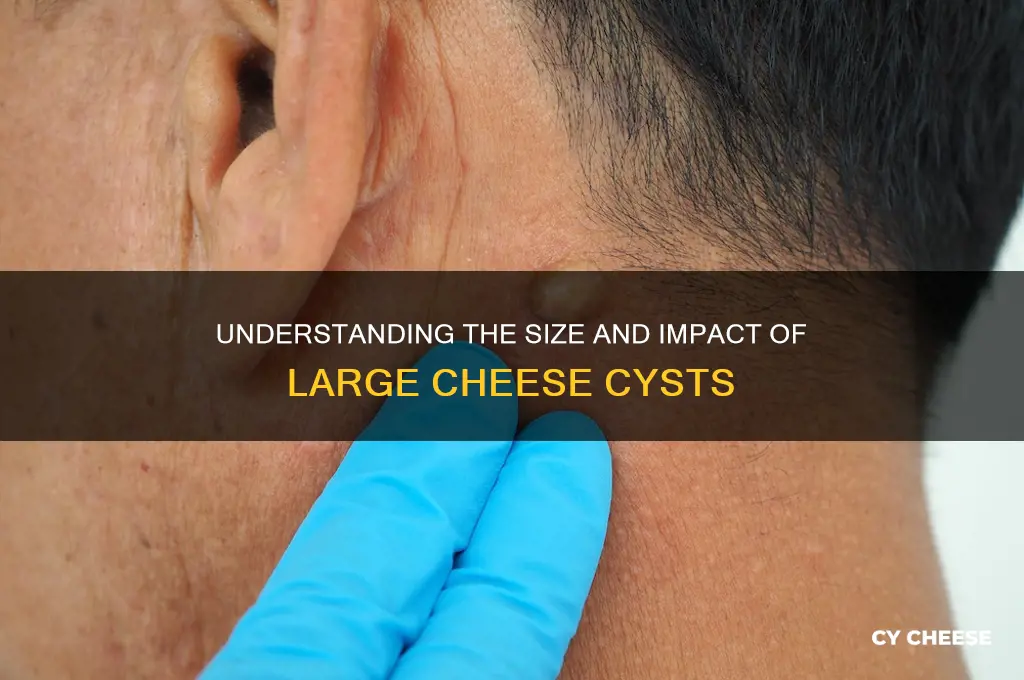
Cheese cysts, more accurately referred to as epidermoid cysts, are benign skin growths that often resemble small lumps filled with a cheese-like material. These cysts form when skin cells move deeper into the skin and multiply, creating a sac filled with keratin, a protein found in skin, hair, and nails. While typically harmless, their size can vary significantly, ranging from a few millimeters to several centimeters in diameter. Understanding the factors influencing their growth, such as location, underlying skin conditions, or trauma, is crucial for determining appropriate management and treatment options.
Explore related products
What You'll Learn
- Symptoms of Large Cheese Cysts: Pain, swelling, redness, and discomfort in affected areas, often accompanied by fever
- Causes of Large Cheese Cysts: Bacterial infections, poor hygiene, or blocked sweat glands leading to cyst formation
- Diagnosis Methods: Physical exams, imaging tests, or fluid analysis to confirm cyst size and type
- Treatment Options: Drainage, antibiotics, or surgical removal to manage large cheese cysts effectively
- Prevention Tips: Maintain hygiene, avoid tight clothing, and treat infections promptly to prevent cyst growth

Symptoms of Large Cheese Cysts: Pain, swelling, redness, and discomfort in affected areas, often accompanied by fever
Large cheese cysts, though a misnomer (they’re actually epidermoid cysts filled with keratin, not cheese), can become problematic when they grow significantly in size. The first symptom to watch for is localized pain, often described as a dull ache or throbbing sensation in the affected area. This pain intensifies with pressure or movement, making it difficult to ignore. For instance, a cyst on the scalp might cause discomfort when brushing hair or wearing a hat, while one on the back could worsen with prolonged sitting. If the cyst is near a nerve, the pain may radiate, mimicking conditions like sciatica or carpal tunnel syndrome.
Swelling and redness are telltale signs that a cyst has grown large enough to irritate surrounding tissues. The skin over the cyst may feel warm to the touch, indicating inflammation. In some cases, the cyst itself becomes visibly distended, forming a firm, round lump beneath the skin. Redness typically spreads outward from the cyst, resembling a target or halo. If the cyst ruptures, the area may swell dramatically as the body reacts to the release of its contents, which can include oily, cheese-like material and dead skin cells.
Discomfort extends beyond pain, encompassing a sense of tightness or heaviness in the affected area. Large cysts can restrict movement, particularly when located in joints or areas with limited space, such as the fingers or wrists. For example, a cyst near the knee might make bending or walking painful, while one on the eyelid could impair vision or cause constant irritation. This discomfort often worsens at night or during physical activity, disrupting daily routines and sleep.
A fever is a critical symptom that suggests the cyst has become infected, a complication more likely with larger cysts due to their increased surface area and potential for rupture. An infected cyst may also drain pus, emit a foul odor, or develop streaks of redness extending from the site. If a fever accompanies other symptoms, seek medical attention promptly. Treatment may involve antibiotics, incision and drainage, or surgical removal to prevent systemic infection or abscess formation.
To manage symptoms at home, apply warm compresses for 10–15 minutes, three times daily, to reduce inflammation and encourage drainage if the cyst is superficial. Avoid squeezing or popping the cyst, as this increases infection risk. Over-the-counter pain relievers like ibuprofen (200–400 mg every 4–6 hours) can alleviate pain and swelling. However, if symptoms persist or worsen, consult a healthcare provider. Large cysts, especially those causing severe pain or fever, often require professional intervention, such as corticosteroid injections or surgical excision, to prevent long-term complications.
Havarti Cheese and Probiotics: Uncovering the Gut-Friendly Truth
You may want to see also

Causes of Large Cheese Cysts: Bacterial infections, poor hygiene, or blocked sweat glands leading to cyst formation
Large cheese cysts, often referred to as epidermoid cysts, can be unsightly and uncomfortable, but understanding their causes is the first step toward prevention and treatment. These cysts are typically filled with a cheese-like material composed of keratin, a protein found in skin cells. While they are generally benign, their size and location can cause concern. The primary culprits behind the formation of large cheese cysts are bacterial infections, poor hygiene, and blocked sweat glands. Each of these factors plays a distinct role in the development of these cysts, and addressing them can help mitigate the risk.
Bacterial infections are a significant contributor to the formation of large cheese cysts. When bacteria, such as *Staphylococcus aureus*, infiltrate the skin through a break or wound, they can trigger inflammation and the accumulation of keratin. This process leads to the formation of a cyst. Individuals with weakened immune systems or those who frequently engage in activities that cause skin trauma, such as contact sports, are particularly susceptible. To reduce the risk, it’s essential to keep wounds clean and covered, and to seek medical attention if signs of infection, such as redness, swelling, or pus, appear. Antibiotics may be prescribed to combat the infection and prevent cyst formation.
Poor hygiene is another critical factor in the development of large cheese cysts. When dead skin cells and oils are not regularly removed, they can accumulate and clog hair follicles or pores, creating an environment conducive to cyst formation. This is especially true in areas prone to sweating and friction, such as the face, neck, and back. Establishing a consistent skincare routine is vital. Cleanse the skin daily with a mild, non-comedogenic cleanser, and exfoliate once or twice a week to remove dead skin cells. For individuals prone to cysts, using products containing salicylic acid or benzoyl peroxide can help prevent blockages. Additionally, wearing breathable fabrics and avoiding tight clothing can reduce friction and sweat buildup.
Blocked sweat glands are a less obvious but equally important cause of large cheese cysts. When sweat glands become obstructed, often due to thick skin or excessive sebum production, sweat and oils can become trapped beneath the skin’s surface. Over time, this can lead to the formation of a cyst. This issue is more common in individuals with oily skin or those who live in humid climates. To prevent blocked sweat glands, it’s crucial to keep the skin dry and clean, particularly after sweating. Using antiperspirants and avoiding heavy moisturizers in prone areas can also help. For existing cysts, warm compresses can encourage drainage, but medical intervention, such as incision and drainage, may be necessary for larger or persistent cases.
In conclusion, large cheese cysts are primarily caused by bacterial infections, poor hygiene, and blocked sweat glands. By understanding these factors, individuals can take proactive steps to prevent cyst formation. Maintaining good hygiene, treating wounds promptly, and keeping the skin clean and dry are practical measures that can significantly reduce the risk. For those already dealing with cysts, medical treatments such as antibiotics, drainage, or surgical removal may be required. Awareness and prevention are key to managing this common skin condition effectively.
Does Lobster Bisque Contain Cheese? Unraveling the Creamy Soup Mystery
You may want to see also

Diagnosis Methods: Physical exams, imaging tests, or fluid analysis to confirm cyst size and type
Cheese cysts, a colloquial term for epidermoid cysts containing keratin that resembles cottage cheese, require precise diagnosis to determine their size, type, and potential complications. Physical exams serve as the initial diagnostic step, where a healthcare provider palpates the cyst to assess its texture, mobility, and tenderness. For instance, a firm, non-tender cyst is more likely to be benign, while redness, swelling, or pain may indicate infection. However, physical exams alone are insufficient for definitive diagnosis, as they cannot confirm internal characteristics or exact size.
Imaging tests, such as ultrasound or MRI, provide detailed insights into cyst structure and dimensions. Ultrasound, a non-invasive and cost-effective option, is ideal for superficial cysts, offering real-time visualization of size, shape, and contents. For deeper or complex cases, MRI excels in distinguishing between cystic and solid masses, with resolution down to millimeters. For example, an MRI can differentiate a 2-cm epidermoid cyst from a sebaceous cyst or abscess, guiding appropriate treatment. These imaging modalities are particularly valuable for cysts in sensitive areas, like the face or spine, where surgical intervention carries higher risks.
Fluid analysis, or aspiration, is another diagnostic tool, especially when infection or malignancy is suspected. A fine-needle aspiration removes a sample of cyst contents for laboratory analysis. Keratinous material, characteristic of cheese cysts, appears as a thick, cheese-like substance under microscopy. However, this method carries risks, such as infection or cyst rupture, and is contraindicated in inflamed or tender cysts. For instance, in a 45-year-old patient with a 3-cm scalp cyst, aspiration confirmed the presence of keratin, ruling out a pilonidal cyst or tumor.
Each diagnostic method has its limitations and best-use scenarios. Physical exams are quick but subjective, imaging tests provide structural detail but may be costly, and fluid analysis offers definitive confirmation but is invasive. For optimal diagnosis, a combination of these methods is often employed. For example, a 20-year-old with a 1.5-cm cyst on the neck might undergo a physical exam followed by ultrasound to measure size and rule out infection, avoiding unnecessary aspiration.
In practice, healthcare providers must tailor the diagnostic approach to the patient’s age, cyst location, and symptoms. For pediatric patients, non-invasive methods like ultrasound are preferred to minimize discomfort. In adults, MRI may be prioritized for deep or recurrent cysts. Practical tips include reassuring patients that most cheese cysts are benign and educating them on signs of infection (e.g., fever, pus) that warrant immediate evaluation. By integrating these methods, clinicians can accurately diagnose cysts, ensuring appropriate management and patient peace of mind.
Cheese on Tacos: A Delicious Debate or Culinary Crime?
You may want to see also
Explore related products

Treatment Options: Drainage, antibiotics, or surgical removal to manage large cheese cysts effectively
Large cheese cysts, often referred to as pilonidal cysts, can cause significant discomfort and require targeted treatment to prevent recurrence. The choice of treatment depends on the cyst’s size, infection status, and the patient’s overall health. Three primary options—drainage, antibiotics, and surgical removal—offer distinct approaches to managing these cysts effectively. Each method has its advantages and limitations, making it essential to tailor the treatment to the individual case.
Drainage is often the first-line treatment for large, infected cheese cysts. This procedure involves numbing the area with a local anesthetic and making a small incision to allow the pus and debris to drain. It provides immediate relief from pain and pressure, but it’s not a permanent solution. Recurrence is common, as drainage doesn’t address the underlying cause of the cyst. Patients should keep the wound clean and follow post-procedure care instructions, such as warm compresses and regular dressing changes. This method is particularly suitable for acute cases where infection is the primary concern.
Antibiotics play a crucial role when the cyst is infected or at risk of infection. Oral antibiotics like cephalexin (500 mg every 6 hours) or clindamycin (300 mg every 8 hours) are commonly prescribed for 7–10 days. For severe infections, intravenous antibiotics may be necessary. However, antibiotics alone are rarely sufficient for long-term management, as they don’t remove the cyst’s contents or structure. They are most effective when paired with drainage or used as a preventive measure after surgical intervention.
Surgical removal is the most definitive treatment for large cheese cysts, particularly for recurrent or chronic cases. Procedures like the Bascom cleft lift or pit picking remove the cyst and surrounding tissue, reducing the likelihood of recurrence. Surgery is typically performed under general anesthesia and may require a short recovery period. While it offers the highest success rate, it’s more invasive and carries risks such as infection, scarring, or prolonged healing. Patients should discuss their medical history and lifestyle with their surgeon to determine the best surgical approach.
In summary, the choice of treatment for large cheese cysts hinges on the cyst’s condition and the patient’s preferences. Drainage provides quick relief but is temporary, antibiotics address infection but not the cyst itself, and surgical removal offers a long-term solution at the cost of invasiveness. A combination of these methods, guided by a healthcare professional, often yields the best outcomes. Early intervention and proper follow-up care are key to managing these cysts effectively.
Does Cream Cheese Cake Need Refrigeration? Storage Tips Revealed
You may want to see also

Prevention Tips: Maintain hygiene, avoid tight clothing, and treat infections promptly to prevent cyst growth
Cheese cysts, often a result of blocked sweat glands or infections, can grow to alarming sizes if left untreated. While some may remain small and harmless, others can expand to several centimeters, causing discomfort and potential complications. Understanding how to prevent their growth is crucial for maintaining skin health and avoiding unnecessary medical interventions.
Maintaining Hygiene: The First Line of Defense
Regular, gentle cleansing is essential to prevent cheese cysts. Use mild, fragrance-free soap and warm water to keep the skin clean, especially in areas prone to sweating, such as the armpits, groin, and under the breasts. For individuals aged 12 and older, incorporating an antibacterial wash twice weekly can reduce bacterial buildup, a common trigger for cyst formation. Avoid harsh scrubbing, as it can irritate the skin and exacerbate the problem. After showering, pat the skin dry instead of rubbing to minimize friction and potential gland blockages.
The Role of Clothing in Cyst Prevention
Tight clothing traps moisture and restricts airflow, creating an ideal environment for cysts to develop. Opt for breathable fabrics like cotton or bamboo, which wick away sweat and allow the skin to breathe. For those who engage in physical activities or live in humid climates, changing out of sweaty clothes promptly is critical. Loose-fitting garments, particularly in areas where cysts commonly occur, can significantly reduce the risk of gland blockages. Consider wearing moisture-wicking undergarments during workouts to keep the skin dry and irritation-free.
Prompt Infection Treatment: A Non-Negotiable Step
Untreated infections are a leading cause of cheese cyst growth. At the first sign of redness, swelling, or pain, apply a warm compress for 10–15 minutes, three times daily, to encourage drainage and reduce inflammation. Over-the-counter topical antibiotics, such as bacitracin or neomycin, can be applied to minor infections, but consult a healthcare provider if symptoms persist beyond 48 hours. For systemic infections, oral antibiotics may be prescribed, typically in a 7–10 day course depending on severity. Ignoring early signs of infection can lead to abscess formation, requiring surgical intervention.
Practical Tips for Long-Term Prevention
Incorporate exfoliation into your skincare routine once a week to remove dead skin cells and prevent gland blockages. For adults, a gentle chemical exfoliant containing salicylic acid can be effective. Avoid sharing personal items like towels or razors to prevent bacterial transfer. If you’re prone to cysts, consider using hypoallergenic deodorants without aluminum or alcohol, as these ingredients can irritate sensitive skin. Lastly, stay hydrated and maintain a balanced diet rich in vitamins A and E, which promote skin health and reduce inflammation.
By prioritizing hygiene, choosing appropriate clothing, and addressing infections swiftly, you can significantly reduce the likelihood of cheese cysts growing to problematic sizes. These proactive measures not only prevent discomfort but also contribute to overall skin wellness.
Does Cheese Increase Mucus? Unraveling the Dairy and Phlegm Myth
You may want to see also
Frequently asked questions
Pilonidal cysts can vary in size, typically ranging from a small pea-sized lump to several centimeters in diameter. Large or chronic cases may form extensive tracts or cavities under the skin.
Pilonidal cysts can enlarge due to repeated irritation, ingrown hairs, or trapped debris. Infections occur when bacteria enter the cyst, leading to swelling, redness, and pus formation, which can increase its size.
Large or infected pilonidal cysts rarely resolve without medical intervention. They often require drainage, antibiotics, or surgical removal to prevent complications like abscesses or recurrent infections.
Treatment options include incision and drainage for infected cysts, antibiotics for infection, and surgical excision (e.g., pilonidal cystectomy) for chronic or large cases. Minimally invasive techniques may also be considered.