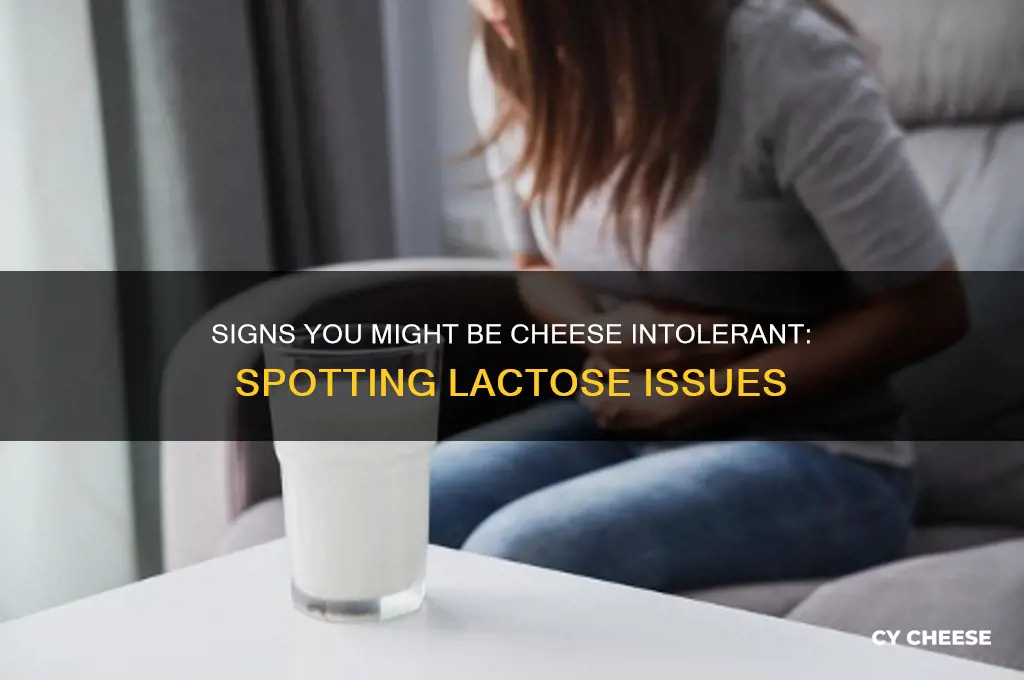
If you suspect you might be intolerant to cheese, it’s important to recognize the signs your body may be giving you. Common symptoms of cheese intolerance include digestive issues like bloating, gas, stomach cramps, or diarrhea, as well as non-digestive symptoms such as headaches, skin rashes, or fatigue. These reactions often occur because cheese contains lactose, a sugar that some people struggle to digest due to insufficient lactase enzymes, or casein, a protein that can trigger sensitivities. Keeping a food diary to track what you eat and any subsequent symptoms can help identify patterns. Additionally, consulting a healthcare professional for tests like a lactose intolerance test or an elimination diet can provide clarity. Understanding your body’s response to cheese is the first step toward managing discomfort and making informed dietary choices.
Explore related products
What You'll Learn

Common Symptoms of Cheese Intolerance
Cheese intolerance often manifests through digestive discomfort, with bloating being a telltale sign. This occurs because the body struggles to break down lactose, a sugar found in cheese, due to insufficient lactase enzymes. If you notice a swollen abdomen after consuming cheese, especially in amounts exceeding 20–30 grams (roughly one slice), this could indicate intolerance. Pairing cheese with lactase supplements or opting for lactose-free varieties may alleviate symptoms, though individual tolerance varies.
Another common symptom is skin reactions, such as hives, itching, or eczema. These occur when the immune system misidentifies proteins in cheese as threats, triggering inflammation. Unlike lactose intolerance, which is digestive, this reaction is immune-mediated and can appear within minutes to hours after consumption. Keeping a food diary to track cheese intake alongside skin changes can help identify patterns. For severe reactions, consult a dermatologist or allergist for patch testing or blood work to confirm the link.
Migraines or headaches post-cheese consumption are less discussed but equally significant. Certain compounds in aged cheeses, like tyramine, can dilate blood vessels, potentially triggering headaches in sensitive individuals. If you experience migraines within 12–24 hours of eating aged cheddar, blue cheese, or Parmesan, tyramine sensitivity might be the culprit. Limiting aged cheeses and opting for fresher varieties like mozzarella or ricotta could reduce symptom frequency.
Lastly, respiratory issues like nasal congestion or wheezing can signal cheese intolerance, particularly if linked to histamine intolerance. Cheese is high in histamine, a compound that can overwhelm the body’s ability to break it down, leading to allergic-like symptoms. Antihistamines may provide temporary relief, but long-term management involves reducing histamine-rich foods. Monitoring symptoms after consuming fermented or aged cheeses can clarify whether histamine is the root cause.
Fontina vs. Fontinella: Unraveling the Differences in These Cheeses
You may want to see also

Lactose vs. Casein Sensitivity Differences
Cheese lovers often find themselves in a quandary when digestive discomfort strikes after indulging in their favorite dairy delight. The culprit could be lactose or casein sensitivity, two distinct conditions with overlapping symptoms but different triggers. Understanding the difference is crucial for managing your diet and well-being.
Symptoms and Timing: A Tell-Tale Sign
Lactose intolerance typically presents with digestive symptoms like bloating, gas, abdominal pain, and diarrhea within 30 minutes to 2 hours after consuming dairy products. This is because the body lacks sufficient lactase, the enzyme needed to break down lactose, a sugar found in milk and cheese. Casein sensitivity, on the other hand, is an immune response to casein, a protein in dairy. Symptoms can be more diverse and may include digestive issues, skin problems like eczema, headaches, and even joint pain. These symptoms often appear hours after consumption and can last longer.
The Elimination Challenge: Pinpointing the Culprit
The most effective way to differentiate between lactose and casein sensitivity is through an elimination diet. Start by completely removing all dairy products from your diet for at least 2-3 weeks. Monitor your symptoms closely during this period. If your symptoms improve significantly, reintroduce dairy products one at a time, starting with lactose-free options like hard cheeses (which have lower lactose content) or lactose-free milk. If symptoms return after consuming these, lactose intolerance is likely the issue. If symptoms persist even with lactose-free dairy, casein sensitivity may be the culprit.
Testing Options: Seeking Professional Guidance
While the elimination diet is a valuable tool, consulting a healthcare professional for proper diagnosis is recommended. They can perform tests like a hydrogen breath test for lactose intolerance, which measures the amount of hydrogen in your breath after consuming a lactose-loaded drink. Elevated hydrogen levels indicate lactose malabsorption. For casein sensitivity, skin prick tests or blood tests for specific antibodies can be helpful, although these tests are not always definitive.
Living with Sensitivity: Navigating the Cheese Aisle
Once you've identified the source of your discomfort, managing your diet becomes easier. For lactose intolerance, opting for lactose-free dairy products, taking lactase enzyme supplements before consuming dairy, or limiting portion sizes can help. Those with casein sensitivity need to strictly avoid all dairy products, including butter, ghee, and even hidden sources like baked goods and processed foods. Fortunately, numerous dairy-free alternatives are available, from plant-based cheeses to nut milks, allowing you to still enjoy delicious and satisfying meals.
Unraveling Amy's Fate in 'I Am the Cheese': A Deep Dive
You may want to see also

Testing Methods for Cheese Intolerance
Cheese intolerance often stems from difficulty digesting lactose or reacting to proteins like casein. Identifying the culprit requires systematic testing, not guesswork. Here’s how to approach it methodically.
Elimination Diet: The Baseline Test
Begin with a dairy-free elimination diet for 2–3 weeks. Exclude all cheese, milk, yogurt, and hidden dairy (e.g., whey in protein powders). Gradually reintroduce small portions of cheese (10–15g, roughly a thumbnail-sized piece) and monitor symptoms over 24–48 hours. Document reactions like bloating, gas, diarrhea, or skin rashes. This method isolates cheese as a trigger but doesn’t pinpoint lactose vs. protein intolerance.
Lactose Breath Test: Measuring Hydrogen Levels
If lactose is the suspect, a hydrogen breath test offers clarity. After fasting overnight, consume a lactose solution (25g lactose in water). Breath samples are collected hourly for 2–5 hours to measure hydrogen levels. Elevated hydrogen indicates undigested lactose fermenting in the gut. This test is 80–90% accurate for lactose malabsorption but doesn’t assess protein intolerance.
Food Allergy vs. Intolerance: Blood Tests
For suspected casein or whey protein intolerance, blood tests like IgE antibody assays or IgG food sensitivity panels can differentiate between allergy and intolerance. IgE tests identify immediate immune reactions (e.g., hives, swelling), while IgG tests highlight delayed responses. However, IgG tests remain controversial, with limited scientific consensus on their reliability. Consult an allergist to interpret results accurately.
Practical Tips for Self-Testing
Hard cheeses (e.g., cheddar, parmesan) naturally contain less lactose due to aging. Start reintroduction trials with these to gauge lactose tolerance. Keep a food diary to correlate symptoms with timing and portion sizes. For children or older adults, consult a dietitian to ensure nutritional needs aren’t compromised during testing.
While self-testing provides insights, persistent or severe symptoms warrant professional evaluation. Combining methods—elimination diet, breath test, and blood work—offers the most comprehensive diagnosis. Understanding your body’s response to cheese empowers tailored dietary choices without unnecessary restrictions.
Unboxing Cheese Nips: Counting the Crunchy Snacks Inside Each Box
You may want to see also
Explore related products

Foods to Avoid if Intolerant
Cheese intolerance often stems from difficulty digesting lactose or reacting to proteins like casein. If you suspect cheese is your culprit, broadening your avoidance strategy to related foods can alleviate symptoms and prevent discomfort. Here’s a targeted guide to navigating dietary restrictions effectively.
Dairy Derivatives: The Obvious and the Hidden
Start by eliminating all dairy products, as they share lactose and proteins with cheese. Milk, butter, yogurt, and ice cream are immediate red flags. Less obvious offenders include cream-based sauces, baked goods (often made with buttermilk or whey), and processed meats like deli ham or sausages, which may contain milk powders as fillers. Even "non-dairy" creamers sometimes harbor casein, so scrutinize labels for terms like "milk solids," "lactose," or "whey."
Fermented Exceptions and Misconceptions
Fermented dairy like kefir or aged cheeses (Parmesan, cheddar) are lower in lactose due to bacterial breakdown. However, protein intolerances won’t be resolved by fermentation. If casein is your trigger, avoid these entirely. Conversely, lactose-intolerant individuals might tolerate small portions of hard cheeses (1–2 ounces) but should still monitor reactions, as tolerance thresholds vary widely.
Cross-Contaminants in Unexpected Places
Cross-contamination lurks in shared equipment or facilities. For instance, dark chocolate often contains milk fat, and protein powders may include whey isolates. Even medications and supplements can use lactose as a binder. Look for "dairy-free" certifications or contact manufacturers for clarity. When dining out, clarify that "no cheese" also means no butter, cream, or hidden dairy in stocks or dressings.
Plant-Based Pitfalls: Not All Substitutes Are Safe
While almond or oat milk cheeses seem safe, some brands add casein for texture. Similarly, vegan pizzas might use shared ovens or utensils, risking trace dairy. Prioritize certified allergen-free facilities and read ingredient lists for additives like "milk protein" or "lactoglobulin." Homemade alternatives (e.g., cashew-based spreads) offer control but require vigilance against cross-contamination in your kitchen.
Long-Term Strategies: Beyond Elimination
After identifying triggers, reintroduce foods systematically to gauge thresholds. For example, test 1/4 cup of lactose-free milk or a casein-free alternative weekly. Keep a symptom journal to track patterns. Consult a dietitian to ensure nutrient balance, as dairy avoidance can lower calcium or vitamin D intake. Supplements or fortified foods (e.g., almond milk with added calcium) can bridge gaps without risking reactions.
By systematically avoiding hidden dairy, understanding fermentation limits, and navigating substitutes wisely, you can manage cheese intolerance without sacrificing flavor or nutrition.
Understanding the Cost Factors Behind a Wheel of Cheese
You may want to see also

Alternatives to Cheese for Intolerant Individuals
Cheese intolerance, often linked to lactose or casein sensitivity, can manifest as bloating, gas, diarrhea, or skin issues. Identifying the culprit is the first step, but the real challenge lies in finding satisfying substitutes. Fortunately, the culinary world offers a plethora of alternatives that mimic cheese’s texture, flavor, or functionality, allowing intolerant individuals to enjoy their favorite dishes without discomfort.
Nut-Based Cheeses: A Creamy, Dairy-Free Delight
For those seeking a rich, spreadable option, nut-based cheeses are a standout. Cashew and macadamia nuts, when blended with probiotic cultures and aged, create a creamy texture reminiscent of soft cheeses like Brie or cream cheese. Brands like Kite Hill offer pre-made versions, but DIY enthusiasts can experiment at home. Start by soaking 2 cups of raw cashews for 4 hours, blending with 2 tablespoons of nutritional yeast, 1 tablespoon of lemon juice, and a pinch of salt. Ferment for 24–48 hours for a tangy kick. These alternatives are ideal for vegan charcuterie boards or as a base for dairy-free sauces.
Coconut-Based Options: Hard and Sliceable
For a firmer, sliceable cheese alternative, coconut-based products shine. Made from coconut milk or oil, these cheeses often include starches like tapioca to achieve a meltable consistency. Violife and Daiya are popular brands offering shredded and block varieties perfect for sandwiches, pizzas, or grilled cheese. While coconut’s flavor can be subtle, it’s best paired with strong seasonings like garlic or smoked paprika to mask any sweetness. Note: Those with tree nut allergies should verify cross-contamination risks.
Vegetable-Based Innovations: Light and Versatile
For a lower-calorie, nut-free option, vegetable-based cheeses use ingredients like carrots, potatoes, or cauliflower. These alternatives are often blended with nutritional yeast—a deactivated yeast rich in umami flavor and B vitamins—to replicate cheese’s savory profile. A simple recipe involves steaming 2 cups of cauliflower, blending it with ¼ cup nutritional yeast, 2 tablespoons of olive oil, and 1 teaspoon of garlic powder. This mixture can be shaped into rounds and chilled for a snackable, cracker-friendly option. These alternatives are particularly suitable for those monitoring fat intake or seeking allergen-free choices.
Fermented Foods: Tangy and Probiotic-Rich
Beyond direct cheese substitutes, fermented foods like sauerkraut, kimchi, or miso can add a tangy, cheesy flavor to meals. For instance, a dollop of miso paste in soups or spreads provides depth without dairy. Similarly, nutritional yeast—often dubbed “nooch”—can be sprinkled on popcorn, pasta, or roasted vegetables for a cheesy, nutrient-dense boost. These options not only satisfy cravings but also support gut health, a bonus for those whose intolerance stems from digestive issues.
Incorporating these alternatives requires creativity, but the payoff is immense. Whether through nut-based spreads, coconut melts, vegetable blends, or fermented additions, cheese-intolerant individuals can reclaim the joy of flavorful, texture-rich meals without compromise. Experimentation is key—start small, mix and match, and discover which substitutes best suit your palate and dietary needs.
Does Panera Soup Contain Velveeta Cheese? Uncovering the Ingredients
You may want to see also
Frequently asked questions
Symptoms include bloating, gas, stomach pain, diarrhea, nausea, skin rashes, headaches, and fatigue after consuming cheese.
Keep a food diary to track symptoms after eating cheese, or try an elimination diet by removing cheese for a few weeks and reintroducing it to observe reactions.
Not always. While lactose intolerance is due to difficulty digesting lactose (milk sugar), cheese intolerance can also be caused by reactions to proteins like casein or other components in cheese.
It depends on the severity of your intolerance. Some people can tolerate small amounts or opt for lactose-free or aged cheeses, which have lower lactose content.
Symptoms can appear within 30 minutes to a few hours after consumption, depending on the individual and the severity of the intolerance.