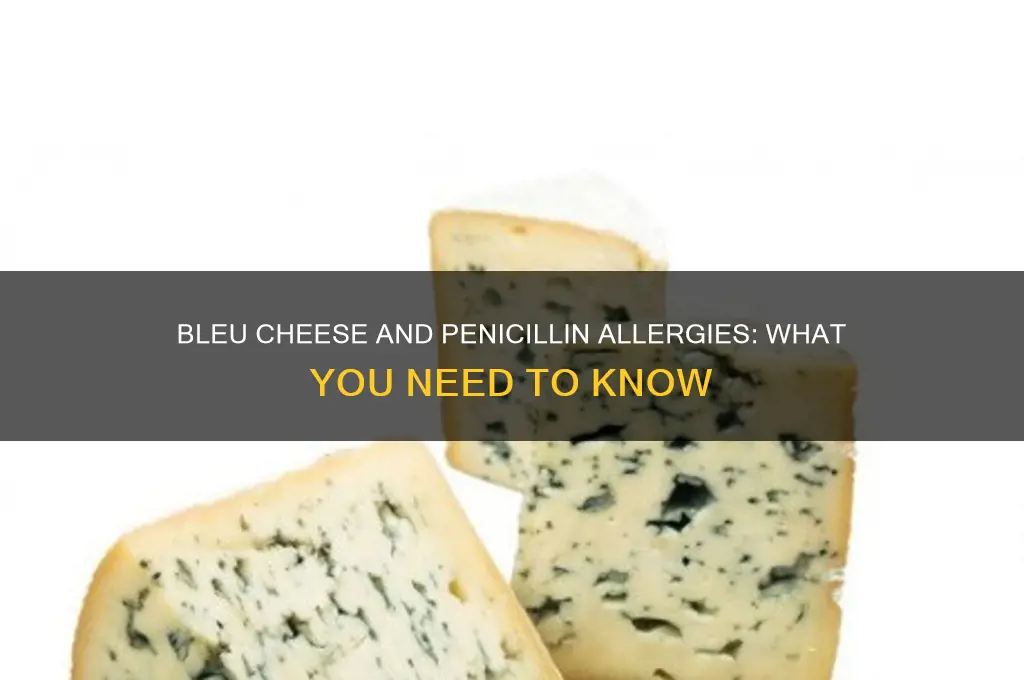
Many people with penicillin allergies wonder if they can safely consume blue cheese, given that certain strains of Penicillium mold are used in its production. While blue cheese is made with Penicillium cultures, the type of mold involved is different from the one used in penicillin antibiotics. However, because cross-reactivity between penicillin and Penicillium-derived foods is rare but possible, individuals with a penicillin allergy should exercise caution. Consulting a healthcare professional is advisable, as they can provide personalized guidance based on the severity of the allergy and individual risk factors.
| Characteristics | Values |
|---|---|
| Cross-Reactivity Risk | Low; most penicillin allergies are caused by specific proteins in the antibiotic, not the mold itself. |
| Mold Type in Blue Cheese | Penicillium roqueforti or Penicillium glaucum, different from Penicillium molds used in penicillin production. |
| Allergic Reaction Risk | Minimal for most penicillin-allergic individuals, but caution is advised due to potential cross-reactivity in rare cases. |
| Medical Advice | Consult a healthcare professional before consuming blue cheese if you have a penicillin allergy. |
| Common Symptoms (if allergic) | Hives, itching, swelling, difficulty breathing, or anaphylaxis (rare). |
| Prevalence of Cross-Reactivity | Less than 1% of penicillin-allergic individuals may react to blue cheese. |
| Safe Alternatives | Non-mold-ripened cheeses (e.g., cheddar, mozzarella) for those concerned about cross-reactivity. |
| Latest Research (as of 2023) | No significant evidence of widespread cross-reactivity between penicillin allergy and blue cheese consumption. |
Explore related products
What You'll Learn

Bleu Cheese vs. Penicillin Mold
Blue cheese, with its distinctive veins of mold, often raises concerns for those with penicillin allergies. The mold in blue cheese, *Penicillium roqueforti*, is a cousin to the *Penicillium* species used in penicillin production, but this familial relation doesn’t automatically mean danger. The key difference lies in the purpose and concentration of the mold. In blue cheese, the mold is cultivated to create flavor and texture, not to produce antibiotics. Penicillin, on the other hand, is a concentrated extract designed to combat bacterial infections. While cross-reactivity is rare, it’s not impossible, making caution advisable for those with severe penicillin allergies.
For individuals with a penicillin allergy, the decision to consume blue cheese should be approached methodically. Start by consulting an allergist to assess the severity of your allergy. Mild reactions, such as hives or itching, may not preclude blue cheese consumption, but severe reactions like anaphylaxis warrant avoidance. If cleared by a medical professional, consider a small taste test under supervision. Monitor for symptoms like swelling, difficulty breathing, or dizziness. If no reaction occurs, gradually increase portion sizes, but always remain vigilant. Practical tip: Keep an epinephrine auto-injector nearby as a precaution.
The science behind penicillin allergies and blue cheese consumption is nuanced. Penicillin allergies are typically triggered by specific proteins in the antibiotic, not the mold itself. Blue cheese contains trace amounts of these proteins, but the risk of reaction depends on individual sensitivity. Studies show that only about 1% of penicillin-allergic individuals react to foods containing *Penicillium* molds. However, this statistic isn’t a guarantee of safety. Age and overall health play a role—older adults or those with compromised immune systems may be more susceptible to reactions. Always prioritize medical advice over general guidelines.
From a comparative standpoint, blue cheese and penicillin mold serve entirely different functions. Penicillin mold is harvested and processed to isolate the antibiotic compound, resulting in a highly concentrated product. Blue cheese, however, uses the mold as part of its fermentation process, leaving behind minimal residual proteins. This distinction is critical for understanding risk. While penicillin is measured in precise dosages (e.g., 250–500 mg capsules), blue cheese consumption is far less controlled. A typical serving (30–50 grams) contains negligible amounts of mold proteins, but the lack of standardization means reactions can vary widely.
In conclusion, blue cheese and penicillin mold share a biological origin but diverge in application and risk. For most penicillin-allergic individuals, blue cheese is likely safe, but caution is paramount. Consult a healthcare provider, start with small amounts, and monitor for adverse reactions. While the mold in blue cheese isn’t a direct threat, the potential for cross-reactivity exists, especially in severe cases. Practical tip: Opt for aged cheeses, as longer aging reduces mold protein content. Knowledge and preparation are your best tools in navigating this culinary conundrum.
What’s a Grilled Cheese Called in the UK? Discover the British Name!
You may want to see also

Cross-Reactivity Risks Explained
Blue cheese, with its distinctive veins of mold, often raises concerns for individuals allergic to penicillin. The worry stems from the fact that both the cheese and the antibiotic share a common fungal origin: Penicillium. However, the critical question is whether this shared lineage translates to cross-reactivity, a phenomenon where an allergy to one substance triggers a reaction to another similar one. Understanding this risk requires a nuanced look at the science behind allergies and the specific proteins involved.
Cross-reactivity occurs when the immune system mistakes a harmless substance for a known allergen due to structural similarities in their proteins. In the case of penicillin allergy, the immune system reacts to specific penicillin-binding proteins or degradation products. Blue cheese, produced with Penicillium molds, contains different proteins and metabolites. Studies suggest that true cross-reactivity between penicillin and blue cheese is extremely rare, with incidence rates below 1%. This is because the proteins in the mold used for cheese production differ significantly from those in the antibiotic.
Despite the low risk, individual sensitivities vary. Some people may experience reactions not due to cross-reactivity but because of histamines or other compounds in aged cheeses. For instance, blue cheese is high in histamine, which can trigger symptoms like headaches or flushing in histamine-intolerant individuals. This is not an allergic reaction but rather a metabolic response. Therefore, it’s essential to distinguish between a true allergy and other forms of intolerance when assessing risk.
If you’re penicillin-allergic and considering blue cheese, start with a small amount to test tolerance. Monitor for symptoms like hives, swelling, or difficulty breathing, which could indicate a rare cross-reaction. Consult an allergist for skin or blood tests if unsure, as they can provide clarity through specific IgE testing. For children or those with severe penicillin allergies, caution is advised, and professional guidance is recommended before introducing blue cheese into the diet.
In summary, while blue cheese and penicillin share a fungal origin, cross-reactivity is uncommon. The risk is minimal for most penicillin-allergic individuals, but personal sensitivities and other factors like histamine intolerance can complicate the picture. Practical steps, such as gradual introduction and medical consultation, can help navigate this safely. Always prioritize expert advice when in doubt, ensuring informed decisions about dietary choices.
Follow Your Heart Cheese: Soy Ingredients Explained for Allergy Concerns
You may want to see also

Safe Consumption Guidelines
Blue cheese, with its distinctive veins of mold, often raises concerns for individuals allergic to penicillin. The key lies in understanding the type of mold involved. Penicillium roqueforti, used in blue cheese production, is a different species from the Penicillium molds that produce penicillin. While cross-reactivity is rare, it’s not impossible. Studies suggest fewer than 1% of penicillin-allergic individuals experience adverse reactions to blue cheese. However, this low risk doesn’t eliminate the possibility entirely, making cautious consumption essential.
For those with a penicillin allergy, a graded exposure approach can help assess tolerance. Start with a small amount, such as a quarter teaspoon of blue cheese, and monitor for symptoms like itching, swelling, or hives over 1–2 hours. If no reaction occurs, gradually increase the portion size over several days. This method allows the body to acclimate while minimizing the risk of a severe allergic response. Always consult an allergist before attempting this, as individual sensitivities vary widely.
Children and the elderly, who may have heightened sensitivities or weaker immune responses, require stricter precautions. For children under 12, avoid introducing blue cheese until their immune systems are more developed. Elderly individuals, particularly those with pre-existing respiratory or immune conditions, should limit consumption to trace amounts, if any. Pregnant or breastfeeding individuals should also exercise caution, as allergic reactions could pose risks to both mother and child.
Practical tips can further mitigate risks. Opt for pasteurized blue cheese, as pasteurization reduces the presence of potentially reactive proteins. Pairing blue cheese with antihistamine-rich foods like citrus or yogurt may also help counteract mild allergic responses. Keep an epinephrine auto-injector nearby when trying blue cheese for the first time, especially if your penicillin allergy is severe. These measures ensure safer exploration of this flavorful cheese while prioritizing health.
Ultimately, while blue cheese is generally safe for most penicillin-allergic individuals, personalized risk assessment is crucial. Factors like allergy severity, age, and overall health play significant roles. When in doubt, err on the side of caution and consult a healthcare professional. Safe consumption isn’t about avoiding enjoyment but about making informed choices that balance indulgence with well-being.
Beyond Velveeta: Top Cheeses to Elevate Your Omelet Game
You may want to see also
Explore related products

Symptoms of Allergic Reactions
Allergic reactions to foods like blue cheese can range from mild to severe, and recognizing the symptoms early is crucial for timely intervention. Mild reactions often manifest as hives, itching, or swelling around the mouth and face. These symptoms typically appear within minutes to an hour after consumption and can usually be managed with over-the-counter antihistamines like diphenhydramine (25–50 mg for adults, 12.5 mg for children aged 6–12). However, if symptoms persist or worsen, seeking medical attention is essential.
In more severe cases, an allergic reaction can escalate to anaphylaxis, a life-threatening condition requiring immediate action. Symptoms of anaphylaxis include difficulty breathing, rapid heartbeat, severe dizziness, and a sudden drop in blood pressure. For individuals at risk, carrying an epinephrine auto-injector (e.g., EpiPen) is critical. Administer the epinephrine immediately upon recognizing symptoms, then call emergency services. The standard dose is 0.3 mg for adults and 0.15 mg for children, injected into the thigh.
Children and the elderly are particularly vulnerable to severe allergic reactions due to their developing or weakened immune systems. Parents and caregivers should monitor for symptoms like persistent coughing, wheezing, or unusual fatigue, which may indicate respiratory distress. For older adults, confusion or a sudden inability to speak clearly can be signs of anaphylaxis. In both age groups, swift action is key—delaying treatment can lead to complications.
To minimize risk, individuals with known penicillin allergies should approach blue cheese cautiously, as it may contain penicillium mold. Cross-reactivity is rare but possible. Practical tips include starting with a small amount (e.g., a crumb-sized portion) and waiting 15–30 minutes to observe any reactions. Keep an antihistamine or epinephrine auto-injector nearby as a precaution. Always consult an allergist for personalized advice, especially if you have a history of severe allergies.
Converting Cheese Cubes to Ounces: A Simple Measurement Guide
You may want to see also

Alternatives to Bleu Cheese
Blue cheese, with its distinctive veins and pungent flavor, is a beloved ingredient in many cuisines. However, for those allergic to penicillin, the concern arises: is it safe to consume? The answer lies in understanding that while blue cheese is made with Penicillium cultures, the type of Penicillium used in cheese production is different from the one in penicillin medication. Still, caution is advised, and exploring alternatives can provide peace of mind.
Analytical Perspective:
For individuals with a penicillin allergy, cross-reactivity with blue cheese is rare but not impossible. Studies suggest that the Penicillium molds in cheese (e.g., Penicillium roqueforti) differ significantly from Penicillium chrysogenum, the source of penicillin. However, since allergic reactions can be unpredictable, substituting blue cheese with similar alternatives is a prudent choice. Options like Gorgonzola, made with Penicillium glaucum, or Cambozola, a blend of Camembert and Gorgonzola, offer comparable flavors without the same mold strain. For a non-mold alternative, consider aged cheddar or Gruyère, which provide a sharp, tangy profile that can mimic blue cheese’s complexity in dishes like salads or pasta.
Instructive Approach:
To replace blue cheese in recipes, start by identifying its role. Is it a crumble for salads, a melt for burgers, or a spread for crackers? For salads, goat cheese or feta provides a tangy, crumbly texture. For melting, try smoked Gouda or Monterey Jack, which add depth without overpowering the dish. If you’re crafting a cheese board, include aged gouda or sharp white cheddar to balance flavors. For dips or spreads, blend cream cheese with garlic, walnuts, and a touch of honey to replicate blue cheese’s creamy, nutty profile. Always taste and adjust seasonings to match the desired intensity.
Persuasive Argument:
Opting for blue cheese alternatives isn’t just about safety—it’s an opportunity to explore new flavors. For instance, Roquefort’s cousin, Fourme d’Ambert, offers a milder, creamier texture that appeals to those wary of strong flavors. Similarly, Stilton, though still a blue cheese, is often better tolerated due to its less pungent profile. For a completely different experience, try vegan blue cheese made from cashews or almonds, which uses non-dairy cultures to achieve a similar veined appearance and tangy taste. These alternatives not only cater to dietary restrictions but also expand culinary horizons.
Comparative Analysis:
While blue cheese is irreplaceable in some dishes, alternatives can come close in specific contexts. For example, in a classic wedge salad, crumbled bacon and ranch dressing can compensate for the absence of blue cheese. In a steak au poivre, a dollop of peppercorn cream sauce provides a bold, spicy contrast akin to blue cheese’s kick. For desserts, pairing pears or honey with a sharp cheddar or aged gouda can mimic the sweet-savory interplay of blue cheese and fruit. Each alternative brings its unique qualities, allowing for creativity without sacrificing flavor.
Descriptive Exploration:
Imagine a cheese board where blue cheese is absent but its spirit remains. Start with a wedge of aged Mimolette, its bright orange hue and nutty flavor commanding attention. Add a slice of creamy Brie for contrast, its soft interior melting on the palate. Include a chunk of smoked cheddar, its smoky aroma evoking warmth. Finish with a sprinkle of toasted pecans and a drizzle of balsamic glaze, creating a symphony of textures and tastes. This arrangement not only avoids blue cheese but also celebrates the diversity of cheeses, proving that alternatives can be just as captivating.
By embracing these alternatives, those with penicillin allergies can enjoy the richness of cheese without compromise, ensuring both safety and satisfaction.
Mastering the Art of the Perfect Cheese Board: Tips and Tricks
You may want to see also
Frequently asked questions
Yes, it is generally safe to eat blue cheese if you're allergic to penicillin. The penicillin produced in blue cheese is in very small amounts and is structurally different from the penicillin used in medications, making it unlikely to trigger an allergic reaction.
While blue cheese contains penicillium mold, the risk of an allergic reaction is very low. The type of penicillin in cheese is not the same as the one used in antibiotics, and most people with penicillin allergies tolerate it without issues.
No, you don’t need to avoid all cheeses. Only blue cheeses and some aged cheeses contain penicillium mold. However, consult your doctor if you have concerns, as individual reactions can vary.
Symptoms of a penicillin allergy include rash, hives, itching, and anaphylaxis. Blue cheese is unlikely to cause these symptoms because the penicillin in cheese is not the same as the medication and is present in minimal amounts.
There is no specific test for blue cheese reactions in penicillin-allergic individuals. However, your doctor may recommend a skin test or oral challenge under medical supervision if you’re unsure about your tolerance.