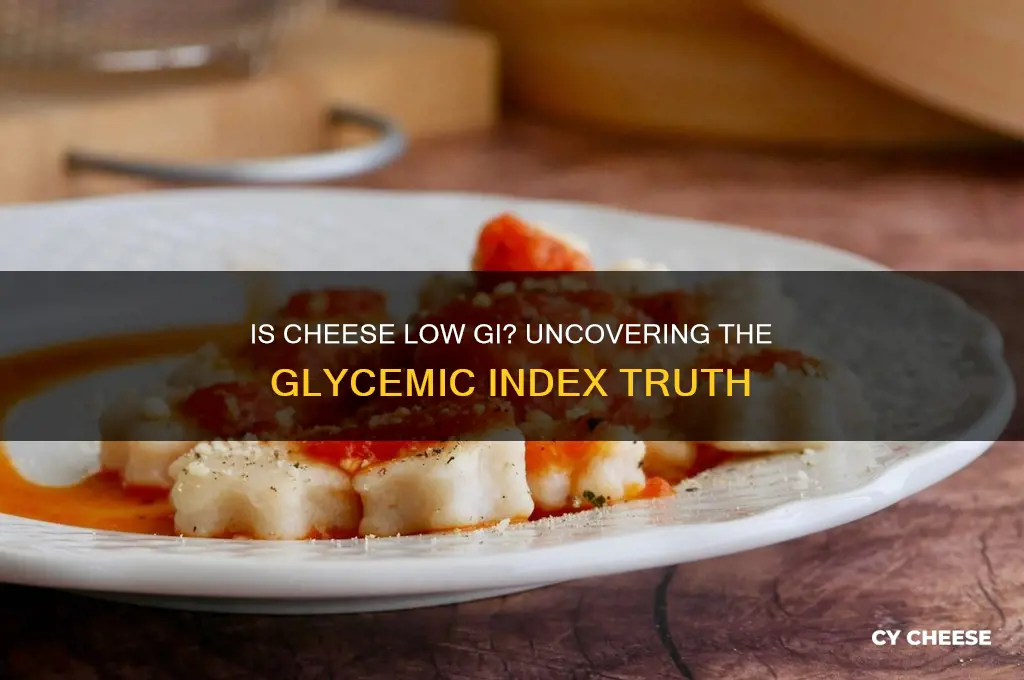
Cheese is a popular food item known for its versatility and rich flavor, but its impact on blood sugar levels is a topic of interest for those monitoring their glycemic index (GI). The GI measures how quickly a food raises blood glucose levels, with low GI foods being preferable for stable energy and better health management. Cheese, being low in carbohydrates and high in fat and protein, generally has a low GI, making it a suitable option for individuals aiming to maintain steady blood sugar levels. However, the specific GI can vary depending on the type of cheese, as factors like fat content and processing methods play a role. Understanding whether cheese is low GI is particularly important for people with diabetes or those following a low-GI diet to support overall well-being.
| Characteristics | Values |
|---|---|
| Glycemic Index (GI) Range | Typically below 15 (very low) |
| Reason for Low GI | Minimal carbohydrate content (less than 5g per serving) |
| Carbohydrate Content | Usually 0-3g per 30g serving |
| Protein Content | High (approx. 6-8g per 30g serving) |
| Fat Content | Moderate to high (approx. 7-12g per 30g serving) |
| Impact on Blood Sugar | Minimal to none due to low carbs and high protein/fat |
| Examples of Low-GI Cheeses | Cheddar, Mozzarella, Swiss, Feta, Goat Cheese |
| Serving Size | Typically 30g (1 ounce) |
| Suitability for Low-GI Diets | Excellent choice due to low GI and nutrient density |
| Additional Benefits | Rich in calcium, vitamin B12, and phosphorus |
Explore related products
$19.99 $24.99
What You'll Learn
- GI Scale Explanation: Understanding the Glycemic Index (GI) scale and its relevance to cheese
- Cheese GI Values: Typical GI values for common cheese types (e.g., cheddar, mozzarella)
- Factors Affecting GI: How fat, protein, and processing impact cheese's GI rating
- Cheese in Diets: Incorporating low-GI cheese into diabetic or weight-management diets
- Comparing Cheese to Other Foods: How cheese's GI compares to bread, fruits, or dairy products

GI Scale Explanation: Understanding the Glycemic Index (GI) scale and its relevance to cheese
The Glycemic Index (GI) is a ranking of carbohydrates on a scale from 0 to 100 based on how quickly and how much they raise blood sugar levels after consumption. Foods with a high GI (70 and above) cause rapid spikes, while those with a low GI (55 and below) release glucose slowly and steadily. Cheese, being primarily composed of protein and fat with minimal carbohydrates, typically falls into the low GI category. For instance, cheddar cheese has a GI value of around 0-10, making it an excellent choice for those monitoring their blood sugar levels.
Understanding the GI scale is particularly relevant for individuals with diabetes or those aiming to manage their weight. Since cheese has a negligible impact on blood glucose, it can be a valuable addition to a low-GI diet. However, not all cheeses are created equal. Processed cheese varieties may contain added sugars or carbohydrates, which could slightly elevate their GI. Always check the nutritional label to ensure the product aligns with your dietary goals. Pairing cheese with high-fiber foods like whole-grain crackers or vegetables can further stabilize blood sugar levels, enhancing its low-GI benefits.
A practical tip for incorporating cheese into a low-GI diet is to focus on natural, minimally processed options like mozzarella, feta, or Swiss cheese. These varieties have virtually no carbohydrates and thus do not significantly affect blood sugar. For example, a 30g serving of mozzarella contains less than 1g of carbs, making it an ideal snack or meal component. Additionally, cheese’s protein and fat content promotes satiety, reducing the likelihood of overeating or reaching for high-GI snacks. This makes it a smart choice for those aiming to maintain stable energy levels throughout the day.
While cheese’s low GI is a clear advantage, it’s essential to consume it in moderation due to its high calorie and fat content. For adults, the American Heart Association recommends limiting saturated fat intake to 5-6% of daily calories. A 30g portion of cheddar cheese, for instance, contains about 6g of fat, primarily saturated. Pairing cheese with low-fat, high-fiber foods can balance its nutritional impact. For children and older adults, portion control is even more critical, as their caloric needs are generally lower. A child’s serving might be half the size of an adult’s, while older adults should focus on nutrient-dense, lower-fat options like part-skim mozzarella.
In conclusion, cheese’s position on the GI scale makes it a favorable food for blood sugar management, but its overall nutritional profile requires mindful consumption. By choosing natural varieties, controlling portions, and pairing it with fiber-rich foods, individuals can harness its low-GI benefits without compromising health. Whether you’re managing diabetes, aiming for weight loss, or simply seeking balanced nutrition, cheese can be a versatile and satisfying addition to your diet when approached thoughtfully.
Hardee's Hot Ham and Cheese: Unveiling the Secret Cheese Blend
You may want to see also

Cheese GI Values: Typical GI values for common cheese types (e.g., cheddar, mozzarella)
Cheese, a staple in many diets, often raises questions about its glycemic index (GI) value, particularly for those monitoring blood sugar levels. The GI measures how quickly a food raises blood glucose, with low GI foods (55 or less) being preferable for steady energy and better blood sugar control. Among common cheese types, most fall into the low GI category, typically ranging between 15 and 30. This is due to their high fat and protein content, which slows carbohydrate absorption. For instance, cheddar cheese, a popular choice, has a GI value of around 20, making it an excellent option for low-GI diets. Similarly, mozzarella, often used in pizzas and salads, also hovers around the same range, ensuring minimal impact on blood sugar levels.
When comparing cheese types, it’s important to note that processing and added ingredients can slightly alter GI values. Natural, minimally processed cheeses like Swiss (GI ~21) and feta (GI ~25) maintain their low GI status. However, cheese spreads or those with added sugars or carbohydrates may have a slightly higher GI. For example, cream cheese, while still low GI (~28), can vary depending on added flavors or sweeteners. For individuals with diabetes or those on a low-GI diet, opting for plain, natural cheeses is advisable. Pairing cheese with high-fiber foods like whole-grain crackers or vegetables can further stabilize blood sugar levels, making it a versatile and practical choice for balanced meals.
From a practical standpoint, incorporating low-GI cheeses into daily meals is straightforward. For breakfast, adding a slice of cheddar to a whole-grain toast provides sustained energy without spiking blood sugar. At lunch, a mozzarella and tomato salad drizzled with olive oil offers a satisfying, low-GI option. For snacks, cubed feta paired with cucumber slices or a handful of nuts combines protein and healthy fats, keeping hunger at bay. Dinner can include grated Swiss cheese melted over steamed vegetables for a nutrient-dense, low-GI side dish. These examples demonstrate how cheese can be a flexible and beneficial component of a low-GI diet, catering to various dietary preferences and needs.
While cheese is generally low GI, portion control remains crucial, especially for calorie-conscious individuals. Cheese is calorie-dense, with a 30g serving of cheddar containing approximately 120 calories. Overconsumption can lead to weight gain, which may indirectly affect blood sugar management. For children, older adults, or those with specific dietary restrictions, consulting a nutritionist can help tailor cheese intake to individual needs. Additionally, combining cheese with other low-GI foods ensures a well-rounded diet. For instance, a snack of apple slices with cheddar provides fiber and protein, promoting satiety and stable blood sugar levels. By understanding GI values and practicing mindful consumption, cheese can be a valuable addition to a healthy, balanced diet.
Are All Cheeses the Same? Unraveling the Dairy Diversity
You may want to see also

Factors Affecting GI: How fat, protein, and processing impact cheese's GI rating
Cheese, a staple in many diets, often raises questions about its glycemic index (GI) rating. While it’s commonly known for its fat and protein content, these very components play a pivotal role in determining its GI. Fat and protein slow down carbohydrate absorption, which is why most cheeses have a low GI. However, not all cheeses are created equal. Factors like fat content, protein levels, and processing methods can subtly shift their GI ratings, making some cheeses more suitable for blood sugar management than others.
Consider the fat content first. Higher-fat cheeses, such as cheddar or Brie, tend to have an even lower GI because fat delays gastric emptying, slowing the release of glucose into the bloodstream. For instance, a 30g serving of full-fat cheddar (with 9g of fat) will have a negligible GI, often listed as 0, compared to a lower-fat option like cottage cheese (with 1g of fat per 100g), which may have a slightly higher GI due to its faster digestion. This doesn’t mean low-fat cheeses are unfavorable—they’re still low GI—but their impact can vary based on fat composition.
Protein content is another critical factor. Cheeses with higher protein levels, like Parmesan or Swiss, further reduce GI by promoting satiety and stabilizing blood sugar. A 30g serving of Parmesan provides around 10g of protein, making it an excellent choice for those monitoring glucose levels. However, protein’s effect is secondary to fat in GI determination, so a high-protein, low-fat cheese like mozzarella (with 22g of protein per 100g) still maintains a low GI primarily due to its fat content.
Processing methods introduce the most variability. Fresh, minimally processed cheeses like ricotta or feta retain their natural fat and protein profiles, ensuring a consistently low GI. In contrast, processed cheeses, often blended with additives and stabilizers, may have altered macronutrient ratios. For example, a processed cheese slice might contain less fat and more carbohydrates (from added ingredients), potentially raising its GI slightly. Always check labels for added sugars or fillers, as these can impact the overall glycemic response.
Practical tip: Opt for full-fat, minimally processed cheeses like cheddar, Brie, or Swiss for the lowest GI. Pair them with high-fiber foods like whole-grain crackers or vegetables to further stabilize blood sugar. Avoid processed cheese products, especially those with added sugars, as they may not offer the same glycemic benefits. By understanding how fat, protein, and processing influence GI, you can make informed choices to align cheese consumption with your dietary goals.
Danish Cheese and Rent: Unraveling the Mystery of Danablu
You may want to see also
Explore related products

Cheese in Diets: Incorporating low-GI cheese into diabetic or weight-management diets
Cheese, often perceived as a high-calorie indulgence, can actually fit into low-GI diets when chosen wisely. The glycemic index (GI) measures how quickly a food raises blood sugar levels, and most cheeses score very low due to their minimal carbohydrate content. For instance, cheddar, mozzarella, and feta typically have a GI of 0–2, making them suitable for diabetics and those managing weight. However, portion control is critical; a 30g serving (about the size of a matchbox) provides flavor without excessive calories or fat. Pairing cheese with high-fiber foods like whole-grain crackers or vegetables further slows sugar absorption, enhancing its low-GI benefits.
Incorporating low-GI cheese into a diabetic diet requires strategic planning. Opt for natural, minimally processed varieties like Swiss or goat cheese, which lack added sugars or preservatives. For weight management, focus on lower-fat options such as cottage cheese or part-skim ricotta, which reduce calorie intake while maintaining satiety. A practical tip is to use cheese as a flavor enhancer rather than the main component of a meal. For example, sprinkle grated parmesan over roasted vegetables or add crumbled feta to a salad for richness without spiking blood sugar or derailing calorie goals.
Comparing cheese to other dairy products highlights its unique role in low-GI diets. Unlike milk or yogurt, which contain lactose and have a higher GI, cheese’s fermentation process removes most carbohydrates, leaving primarily protein and fat. This makes it an ideal snack for stabilizing blood sugar between meals. For instance, a mid-morning snack of 30g of cheddar with a small apple provides sustained energy without the sugar spike associated with sweeter dairy options. However, beware of processed cheese products, which often contain added sugars and fillers, negating their low-GI advantage.
Persuasively, low-GI cheese can be a game-changer for those struggling with cravings during weight loss or blood sugar management. Its high protein and fat content promotes fullness, reducing the urge to snack on high-GI alternatives like chips or cookies. A study published in the *American Journal of Clinical Nutrition* found that participants who included cheese in their low-GI diet experienced greater satiety and better glucose control compared to those on a high-GI plan. To maximize benefits, combine cheese with other low-GI foods like nuts, seeds, or non-starchy vegetables, creating balanced meals that support long-term dietary adherence.
Finally, age-specific considerations are essential when incorporating low-GI cheese into diets. For older adults, calcium-rich cheeses like Swiss or Gruyère support bone health, while younger individuals may prioritize lower-fat options for weight maintenance. Children can benefit from small servings of mild cheeses like mozzarella or string cheese as part of a balanced diet, but moderation is key to avoid excessive saturated fat intake. Regardless of age, consulting a dietitian ensures cheese is integrated safely and effectively into individualized meal plans, aligning with specific health goals and nutritional needs.
Quarter Pounder with Cheese Meal: Uncovering Its Point Value
You may want to see also

Comparing Cheese to Other Foods: How cheese's GI compares to bread, fruits, or dairy products
Cheese, a staple in many diets, often raises questions about its glycemic index (GI) compared to other common foods. The GI measures how quickly a food raises blood sugar levels, with low GI foods (55 or less) being ideal for steady energy and better blood sugar control. Cheese, being low in carbohydrates, typically has a GI of 0, making it a favorable choice for those monitoring their glucose levels. But how does it stack up against bread, fruits, or other dairy products? Let’s break it down.
Consider bread, a carbohydrate-rich food that varies widely in GI depending on its type. White bread, for instance, has a high GI of around 75, causing rapid spikes in blood sugar. Whole grain bread fares better, with a GI of approximately 51, but it still contains more carbs than cheese. For someone aiming to stabilize blood sugar, pairing cheese with whole grain bread can mitigate the bread’s impact, as the fat and protein in cheese slow digestion. However, cheese alone remains the lower GI option, making it a smarter standalone snack for glycemic control.
Fruits, often praised for their nutritional benefits, present an interesting contrast. While fruits like apples (GI of 38) and berries (GI of 25–40) are low GI, others like watermelon (GI of 72) and pineapple (GI of 66) can cause quicker blood sugar spikes. Cheese, with its negligible GI, offers a stable alternative for those sensitive to sugar fluctuations. For a balanced snack, combining low-GI fruits like berries with cheese can provide fiber, vitamins, and sustained energy without the sugar crash.
Among dairy products, cheese stands out for its minimal impact on blood sugar. Milk, for example, has a GI of around 30–40, depending on its fat content, due to the natural sugars lactose and galactose. Yogurt, particularly flavored varieties with added sugar, can have a GI of 35–50. While these dairy options are still relatively low GI, cheese’s lack of carbohydrates gives it an edge for those strictly managing glucose levels. Opting for cheese over sweetened yogurt or a glass of milk can be a strategic choice for low-GI diets.
In practical terms, understanding these comparisons allows for smarter food choices. For a low-GI breakfast, swap a bagel (GI of 72) for a slice of whole grain toast with cheese. For dessert, choose a cube of cheese over a high-GI fruit like mango (GI of 51). When snacking, pair cheese with low-GI fruits or nuts instead of crackers. By leveraging cheese’s unique GI profile, individuals can enjoy a versatile, satisfying food while maintaining stable blood sugar levels.
Understanding the Legal Labeling Requirements for Grass-Fed Cheese Products
You may want to see also
Frequently asked questions
"Low GI" refers to a food having a low glycemic index, meaning it causes a slower and smaller rise in blood sugar levels compared to high-GI foods.
Yes, cheese is generally considered a low GI food because it contains minimal carbohydrates and is high in fat and protein, which do not significantly impact blood sugar levels.
The GI of cheese remains low regardless of type, as most cheeses have negligible carbohydrates. However, processed cheeses with added ingredients might have slightly different nutritional profiles.
Yes, cheese can be included in a low GI diet for people with diabetes, as it does not cause rapid spikes in blood sugar. However, portion control is important due to its high calorie and fat content.
Cheese itself is inherently low GI, but if paired with high-GI foods (e.g., crackers or bread), the overall glycemic impact of the meal may increase.