Lactose intolerance is a common digestive condition where the body lacks sufficient lactase, the enzyme needed to break down lactose, a sugar found in milk and dairy products. While many assume lactose intolerance affects all dairy equally, some individuals report symptoms only after consuming specific dairy items, particularly cheese. This raises the question: is it possible to be lactose intolerant to just cheese? Cheese generally contains less lactose than milk due to the fermentation process, which breaks down much of the lactose. However, certain cheeses, like fresh cheeses (e.g., mozzarella or ricotta), retain higher lactose levels, potentially triggering symptoms in sensitive individuals. Additionally, factors like portion size, individual tolerance thresholds, and the presence of other dairy sensitivities could contribute to cheese-specific reactions. Understanding these nuances can help clarify why some people may experience discomfort only with cheese while tolerating other dairy products.
| Characteristics | Values |
|---|---|
| Possibility of Cheese-Specific Intolerance | Yes, it is possible to be intolerant to cheese but not other dairy products. |
| Reason | Cheese contains less lactose than milk, but some individuals may still react due to sensitivity to small amounts of lactose or other components like casein, histamine, or fermentation byproducts. |
| Lactose Content in Cheese | Hard cheeses (e.g., cheddar, Swiss) have very low lactose (<1g per serving), while soft cheeses (e.g., cream cheese, ricotta) contain more lactose. |
| Other Potential Triggers | Histamine (found in aged cheeses), casein (milk protein), or additives in processed cheeses can cause symptoms similar to lactose intolerance. |
| Symptoms | Bloating, gas, diarrhea, abdominal pain, nausea, after consuming cheese. Symptoms may vary in severity depending on individual tolerance. |
| Diagnosis | Elimination diet, lactose tolerance test, or breath test can help identify lactose intolerance. Additional testing may be needed to rule out other triggers like histamine or casein sensitivity. |
| Management | Avoid or limit cheese, especially soft or processed varieties. Opt for lactose-free cheese or hard cheeses with minimal lactose. Lactase enzymes may help in some cases. |
| Prevalence | Lactose intolerance affects ~65% of the global population, but cheese-specific intolerance is less common and varies by individual. |
| Genetic Factors | Lactose intolerance is often genetic, with higher prevalence in certain populations (e.g., Asians, Africans, Native Americans). |
| Misconception | Not all dairy intolerance is due to lactose. Reactions to cheese could stem from other dairy components, not just lactose. |
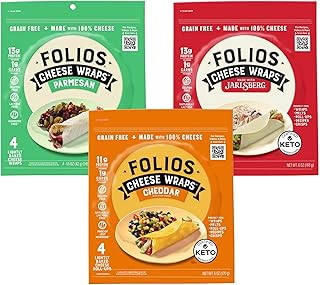
Explore related products
What You'll Learn
- Cheese vs. Milk Lactose Content: Cheese has less lactose than milk; intolerance severity varies by type
- Aged Cheese Tolerance: Harder, aged cheeses have lower lactose, often easier to digest
- Individual Sensitivity Levels: Some may tolerate milk but react to cheese due to personal thresholds
- Fermentation Impact: Fermented cheeses like cheddar reduce lactose, aiding digestion for some
- Other Dairy Components: Intolerance might stem from proteins or fats, not just lactose

Cheese vs. Milk Lactose Content: Cheese has less lactose than milk; intolerance severity varies by type
Cheese generally contains less lactose than milk, making it a more tolerable option for many with lactose intolerance. For instance, a cup of whole milk contains about 12 grams of lactose, while a 1.5-ounce serving of cheddar cheese has less than 0.5 grams. This significant difference stems from the cheese-making process, where lactose is largely removed with the whey. However, the lactose content in cheese varies by type: fresh cheeses like ricotta or mozzarella retain more lactose, while aged cheeses like Parmesan or Swiss have minimal amounts. Understanding these variations can help individuals with lactose intolerance navigate dairy consumption more effectively.
Analyzing lactose intolerance severity requires considering both the lactose content and the portion size consumed. For example, while hard cheeses like Gruyère contain negligible lactose (less than 0.1 grams per ounce), eating a large serving could still trigger symptoms in highly sensitive individuals. Soft, creamy cheeses like Brie or Camembert, though lower in lactose than milk, may still cause discomfort due to their higher lactose levels compared to aged varieties. Keeping a food diary to track symptoms and portion sizes can help identify personal tolerance thresholds. This approach allows for a more nuanced understanding of how different cheeses affect individual digestive systems.
For those experimenting with cheese consumption, start with small portions of aged, hard cheeses to minimize risk. Gradually introduce softer cheeses in modest amounts to gauge tolerance. Pairing cheese with other foods can also slow digestion, potentially reducing lactose-related symptoms. Practical tips include opting for lactose-free cheese alternatives or taking lactase enzymes before meals containing dairy. Age plays a role too: lactose intolerance often develops in adulthood, so younger individuals may tolerate cheese better than older adults. Tailoring cheese choices to personal tolerance levels ensures enjoyment without discomfort.
Comparing cheese and milk highlights why some lactose-intolerant individuals tolerate cheese but not milk. Milk’s high lactose content (11–13 grams per cup) makes it a common trigger, whereas the fermentation and aging processes in cheese production drastically reduce lactose. For example, blue cheese or Gouda contains less than 0.1 grams of lactose per ounce, making them safer options. However, individual sensitivity varies, and some may still react to trace amounts in cheese. This comparison underscores the importance of selecting cheeses based on their lactose content and personal tolerance, rather than avoiding dairy entirely.
Persuasively, the science behind cheese’s lower lactose content offers a compelling case for its inclusion in lactose-intolerant diets. Studies show that aged cheeses, with their minimal lactose, are well-tolerated by up to 80% of lactose-intolerant individuals. This contrasts sharply with milk, which often causes symptoms in the same population. By choosing low-lactose cheeses, individuals can enjoy dairy’s nutritional benefits—calcium, protein, and vitamins—without adverse effects. This evidence-based approach empowers people to make informed dietary choices, debunking the myth that lactose intolerance means complete dairy avoidance.
Mastering Creighton the Wanderer: Cheesing Strategies for Siris' Fight
You may want to see also

Aged Cheese Tolerance: Harder, aged cheeses have lower lactose, often easier to digest
Lactose intolerance often manifests as a blanket sensitivity to dairy, but the reality is more nuanced. For those who find themselves uncomfortable after a slice of cheddar yet unaffected by a splash of milk in coffee, the culprit might be the type of dairy, not dairy itself. Aged, harder cheeses like Parmesan, Pecorino, or aged Gouda undergo a natural aging process that significantly reduces their lactose content. This transformation occurs as bacteria break down lactose into lactic acid, leaving behind a cheese with less than 2 grams of lactose per 100 grams—a threshold often tolerable even for many lactose-intolerant individuals.
Consider the aging process as a natural filtration system. Fresh cheeses like mozzarella or ricotta retain much of their lactose, typically containing 3–5 grams per 100 grams, making them more likely to trigger digestive discomfort. In contrast, a year-aged cheddar or a two-year-old Parmesan can have lactose levels as low as 0.1 grams per 100 grams. For context, most lactose-intolerant individuals can handle up to 12 grams of lactose daily without symptoms, though this varies widely. Starting with small portions—say, 10–20 grams of aged cheese—can help gauge tolerance.
Practical tips for experimenting with aged cheeses include pairing them with enzymes like lactase supplements or incorporating them into meals with other foods to slow digestion. For instance, a few cubes of aged Gruyère in a salad or a sprinkle of grated Parmesan on pasta may be better tolerated than eating the cheese alone. Keep a food diary to track portion sizes and symptoms, as individual thresholds differ. For those with severe intolerance, even trace lactose can cause issues, but for many, aged cheeses offer a delicious loophole.
The science behind this lies in the role of bacteria during aging. As cheeses harden and lose moisture, lactose is metabolized, and the texture becomes denser. This process not only reduces lactose but also concentrates flavor, explaining why aged cheeses are often sharper and more intense. For example, a young cheddar aged 6 months may still contain 2–3 grams of lactose, while a 24-month version drops below 1 gram. This makes longer-aged varieties a safer bet for those testing their limits.
Ultimately, aged cheeses are not a cure for lactose intolerance but a strategic workaround. They allow individuals to enjoy dairy’s richness without the discomfort, provided they choose wisely and listen to their bodies. Start small, experiment gradually, and savor the complexity of a well-aged cheese—it’s a testament to both biology and culinary craft.
Mastering the Art of Arranging a Cheese Platter à la Ina Garten
You may want to see also

Individual Sensitivity Levels: Some may tolerate milk but react to cheese due to personal thresholds
Lactose intolerance manifests differently across individuals, and the idea that someone might tolerate milk but react adversely to cheese isn’t as paradoxical as it seems. Cheese, despite being a dairy product, typically contains less lactose than milk due to the fermentation process. For instance, a cup of milk contains around 12 grams of lactose, while a 30-gram serving of cheddar cheese contains less than 0.5 grams. However, even this small amount can trigger symptoms in highly sensitive individuals. The key lies in personal lactose thresholds, which vary widely based on factors like age, genetics, and gut health.
Consider a scenario where a person consumes a glass of milk without issue but experiences bloating after eating a slice of cheese. This discrepancy could stem from the concentration of lactose per bite rather than the total amount consumed. Cheese, being denser and often consumed in smaller portions, delivers lactose in a more concentrated form. For someone with a low tolerance threshold, this concentration can overwhelm their lactase enzyme capacity, leading to discomfort. Tracking symptoms after specific dairy products can help identify these thresholds, allowing for better dietary management.
Age plays a significant role in this dynamic, as lactase production naturally declines over time. A 30-year-old might tolerate milk but react to cheese due to their reduced enzyme activity, while a teenager with the same sensitivity might handle both without issue. Practical tips include starting with small portions of cheese and pairing it with other foods to dilute lactose concentration. Over-the-counter lactase enzymes can also be taken before consuming dairy to mitigate reactions, though effectiveness varies by individual.
Comparatively, hard cheeses like Parmesan or Swiss are better tolerated than softer varieties like mozzarella or brie, as harder cheeses undergo longer aging processes that break down more lactose. For example, a 30-gram serving of Swiss cheese contains less than 1 gram of lactose, making it a safer option for those with moderate sensitivities. Experimenting with different types of cheese and monitoring reactions can help pinpoint which varieties align with personal thresholds.
Ultimately, understanding individual sensitivity levels requires a personalized approach. Keeping a food diary to record dairy consumption and symptoms can provide clarity. For those who tolerate milk but not cheese, the solution might lie in choosing low-lactose cheeses or adjusting portion sizes. This tailored strategy ensures that dietary restrictions are as minimal as possible while maintaining comfort and health.
Quarter Pounder Without Cheese: Is It Possible to Order?
You may want to see also
Explore related products

Fermentation Impact: Fermented cheeses like cheddar reduce lactose, aiding digestion for some
Fermented cheeses like cheddar undergo a transformation that significantly reduces their lactose content, making them more digestible for individuals with lactose intolerance. During the fermentation process, bacteria convert lactose into lactic acid, breaking down much of the sugar that typically causes digestive discomfort. For example, a 30-gram serving of aged cheddar contains less than 0.5 grams of lactose, compared to fresh cheeses like ricotta, which can contain up to 3 grams per serving. This reduction explains why some people who struggle with milk or ice cream may tolerate cheddar without issue.
To maximize the benefits of fermented cheeses, consider the aging process. The longer a cheese is aged, the more lactose is broken down. Hard cheeses like Parmesan, aged for at least 12 months, often contain negligible amounts of lactose, typically below 0.1 grams per serving. Semi-hard cheeses like Swiss or Gouda, aged for 4–10 months, also have reduced lactose levels but may still contain trace amounts. For those with mild lactose intolerance, starting with small portions (15–20 grams) of aged cheeses can help gauge tolerance before increasing intake.
Not all fermented cheeses are created equal, and individual responses can vary. While cheddar and Parmesan are generally well-tolerated, blue cheeses like Gorgonzola or Roquefort may still pose issues due to their higher lactose content and mold-induced fermentation processes. Additionally, lactose intolerance severity plays a role. People with mild intolerance may handle fermented cheeses easily, while those with severe intolerance might still experience symptoms. Pairing cheese with lactase enzymes or consuming it alongside other foods can further aid digestion.
Practical tips for incorporating fermented cheeses into a lactose-intolerant diet include experimenting with varieties and portion sizes. Keep a food diary to track which cheeses and amounts work best for you. Opt for harder, longer-aged cheeses when possible, and avoid soft, fresh cheeses unless they’re explicitly labeled lactose-free. For social situations, carry lactase supplements as a backup. Over time, understanding your body’s response to fermented cheeses can expand your dietary options without sacrificing comfort.
Chihuahua Cheese vs. Queso Fresco: Unraveling the Dairy Difference
You may want to see also

Other Dairy Components: Intolerance might stem from proteins or fats, not just lactose
Lactose intolerance often steals the spotlight, but dairy discomfort can arise from other culprits lurking in milk products. Beyond the sugar, proteins like casein and whey, as well as milk fats, can trigger digestive distress in sensitive individuals. This means someone might tolerate lactose-free milk but still react to cheese, yogurt, or butter due to these other components. Understanding this distinction is crucial for pinpointing the true source of dairy-related symptoms.
Consider the case of casein, a protein found in high concentrations in cheese. For those with a casein sensitivity, even small amounts can lead to bloating, gas, or diarrhea. Unlike lactose intolerance, which typically manifests as gas and bloating within 30 minutes to 2 hours of consumption, casein reactions can be delayed, making them harder to identify. Keeping a food diary and noting symptoms can help uncover patterns, especially if cheese seems to be a consistent trigger despite lactose-free choices.
Milk fats, though less commonly problematic, can also cause issues. Individuals with conditions like gallbladder dysfunction or fat malabsorption may struggle to digest the high fat content in cheese, leading to symptoms like nausea, abdominal pain, or greasy stools. Interestingly, butter, which is almost purely fat, might be better tolerated than cheese due to its lower protein content. Experimenting with low-fat dairy options or consulting a dietitian can help determine if fats are the culprit.
For those suspecting a non-lactose dairy intolerance, an elimination diet is a practical first step. Start by removing all dairy for 2–3 weeks, then reintroduce specific items one at a time, noting reactions. Begin with lactose-free milk to rule out lactose, then test cheese, yogurt, and butter separately. This methodical approach can isolate whether proteins, fats, or lactose are the true offenders. Pairing this with medical advice, such as allergy testing or breath tests, ensures a comprehensive diagnosis.
Armed with this knowledge, individuals can tailor their diets to avoid specific triggers while still enjoying dairy alternatives. For instance, someone sensitive to casein might opt for ghee (clarified butter with removed milk solids) or plant-based cheeses. Those with fat intolerance could choose low-fat dairy or rely on lactose-free options. By focusing on the lesser-known components of dairy, people can navigate their dietary restrictions with greater precision and fewer sacrifices.
Vegan vs. Regular Cheese: Which is Healthier for You?
You may want to see also
Frequently asked questions
Yes, it’s possible. Some people may tolerate lactose in milk or yogurt but react to cheese, especially aged or hard varieties, due to differences in lactose content or other components like histamine.
Cheese generally contains less lactose than milk, but aged cheeses have even lower levels. However, some cheeses may still trigger symptoms due to individual sensitivity thresholds or the presence of other compounds like histamine.
Absolutely. Harder, aged cheeses like cheddar or Parmesan have very little lactose, while softer, fresher cheeses like mozzarella or cream cheese contain more. Symptoms may be more pronounced with higher-lactose cheeses.