The question of whether consuming too much cheese can lead to bad acid is rooted in the interplay between diet and digestive health. Cheese, a dairy product rich in fat and protein, can be difficult to digest for some individuals, particularly those with lactose intolerance or sensitivity to dairy. When consumed in excess, cheese may contribute to acid reflux, bloating, or gastrointestinal discomfort due to its high fat content and potential to stimulate stomach acid production. Additionally, the term bad acid might refer to an imbalance in gut pH or the overproduction of stomach acid, which can be exacerbated by heavy cheese consumption. While moderate cheese intake is generally safe for most people, overindulgence may lead to digestive issues, highlighting the importance of mindful consumption and awareness of one's dietary tolerances.
| Characteristics | Values |
|---|---|
| Nutrient Density | Cheese is high in calcium, protein, and vitamins like B12 and A, but excessive consumption can lead to nutrient imbalances. |
| Fat Content | High in saturated fats, which may increase LDL ("bad") cholesterol and cardiovascular risk when consumed in excess. |
| Sodium Content | Cheese is high in sodium, which can contribute to hypertension and kidney issues if consumed excessively. |
| Caloric Density | High in calories, potentially leading to weight gain if portion sizes are not controlled. |
| Lactose Content | Contains lactose, which may cause digestive issues in lactose-intolerant individuals. |
| Acid Production | Cheese is not inherently acidic, but excessive consumption can lead to acid reflux or heartburn in some individuals due to high fat content. |
| Gut Health | Contains probiotics in fermented varieties (e.g., cheddar, Swiss), but overconsumption may disrupt gut balance. |
| Allergenic Potential | Contains dairy proteins (casein, whey), which can trigger allergies or sensitivities in some people. |
| Recommended Intake | Moderation is key; 1-2 servings (1.5-2 oz) per day is generally considered safe for most individuals. |
| Health Risks | Excessive intake may contribute to obesity, heart disease, and kidney stones due to high fat, sodium, and phosphorus content. |
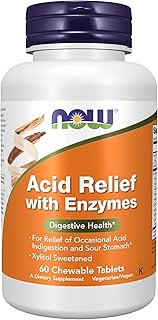
Explore related products
$13.21 $21
What You'll Learn
- Cheese and Acid Reflux: High-fat cheese can relax the esophageal sphincter, worsening acid reflux symptoms
- Lactose Intolerance Impact: Excess cheese may trigger acid production in lactose-intolerant individuals due to undigested lactose
- Saturated Fat Concerns: Cheese's saturated fat content can stimulate stomach acid secretion, potentially causing discomfort
- Fermented Cheese Effects: Aged cheeses may reduce acid issues due to lower lactose and easier digestion
- Portion Control Tips: Limiting cheese intake and pairing with alkaline foods can minimize acid-related problems

Cheese and Acid Reflux: High-fat cheese can relax the esophageal sphincter, worsening acid reflux symptoms
High-fat cheese can be a silent saboteur for those prone to acid reflux. The culprit lies in its ability to relax the lower esophageal sphincter (LES), a muscular valve that acts as a barrier between the stomach and esophagus. When the LES weakens, stomach acid can flow backward, causing the burning sensation and discomfort characteristic of acid reflux. This isn't just anecdotal; studies have shown a correlation between high-fat diets and increased acid reflux symptoms.
Consider this scenario: a 40-year-old with a history of occasional heartburn indulges in a late-night cheese platter featuring sharp cheddar, brie, and blue cheese. All three are high in fat, with cheddar containing around 9 grams of fat per ounce. This fatty feast can trigger a cascade of events: the LES relaxes, stomach acid rises, and within hours, they're reaching for antacids. The takeaway? Portion control is key. Limiting high-fat cheese to 1-2 ounces per serving and avoiding it close to bedtime can significantly reduce the risk of nighttime reflux.
Not all cheeses are created equal in their reflux-inducing potential. Opting for lower-fat varieties like part-skim mozzarella (4 grams of fat per ounce) or fresh goat cheese (6 grams of fat per ounce) can be a smarter choice for acid reflux sufferers. Pairing cheese with fiber-rich foods like whole-grain crackers or vegetables can also help slow digestion, reducing the likelihood of acid backflow. For those with severe reflux, consulting a dietitian to create a personalized low-fat cheese plan might be beneficial.
While cheese can be a dietary landmine for acid reflux, it doesn't necessitate complete avoidance. Moderation, mindful selection, and strategic timing are the pillars of enjoying cheese without paying the price later. For instance, incorporating cheese into a balanced lunch rather than as a late-night snack can minimize its impact on the LES. Additionally, keeping a food diary to track cheese intake and reflux episodes can help identify individual triggers and thresholds.
In conclusion, the relationship between high-fat cheese and acid reflux is rooted in its effect on the esophageal sphincter. By understanding this mechanism and adopting practical strategies—such as choosing lower-fat options, controlling portions, and timing consumption—individuals can savor cheese without exacerbating their symptoms. It's not about deprivation but informed indulgence.
Phosphorus Content in a Slice of American Cheese: A Nutritional Breakdown
You may want to see also

Lactose Intolerance Impact: Excess cheese may trigger acid production in lactose-intolerant individuals due to undigested lactose
Excessive cheese consumption can spell trouble for those with lactose intolerance, a condition affecting approximately 68% of the global population. When lactose-intolerant individuals consume dairy products like cheese, their bodies lack sufficient lactase, the enzyme needed to break down lactose, a sugar found in milk. This undigested lactose ferments in the gut, producing gas, bloating, and discomfort. However, a lesser-known consequence is its impact on stomach acid production. The fermentation process triggers the release of short-chain fatty acids, which can stimulate gastric acid secretion, leading to symptoms like heartburn or acid reflux.
Consider a scenario where a lactose-intolerant adult consumes 50 grams of cheddar cheese (roughly 2 slices), which contains about 0.5 grams of lactose. While this amount might be tolerable for some, exceeding this threshold—say, by adding another 50 grams—can overwhelm the digestive system. The undigested lactose acts as a substrate for gut bacteria, accelerating acid production. For context, the average lactose intolerance threshold is around 12 grams of lactose per sitting, but individual tolerance varies widely. Monitoring portion sizes and opting for low-lactose cheeses like Swiss or aged cheddar can mitigate this risk.
From a practical standpoint, managing acid-related symptoms in lactose-intolerant individuals requires a two-pronged approach. First, limit cheese intake to small, measured portions, especially during meals. Pairing cheese with lactase supplements, such as Lactaid, can aid lactose digestion and reduce acid triggers. Second, incorporate acid-neutralizing strategies, like consuming alkaline foods (e.g., bananas or ginger) or over-the-counter antacids, to counteract excess stomach acid. For chronic sufferers, consulting a dietitian to design a low-lactose, low-acid meal plan can provide long-term relief.
Comparatively, lactose-intolerant individuals often fare better with fermented dairy products like yogurt or kefir, which contain live cultures that assist in lactose breakdown. However, cheese, particularly fresh varieties like mozzarella or ricotta, retains higher lactose levels due to shorter aging times. Aged cheeses, on the other hand, undergo a natural process that reduces lactose content, making them a safer option. For instance, 30 grams of Parmesan contains less than 0.05 grams of lactose, making it a viable choice for those with mild intolerance. Understanding these differences empowers individuals to make informed dietary choices.
Ultimately, the link between excess cheese and acid production in lactose-intolerant individuals underscores the importance of personalized dietary management. While cheese can be a nutritious addition to the diet, its lactose content demands caution. By balancing intake, selecting low-lactose options, and employing digestive aids, individuals can enjoy cheese without triggering discomfort. Awareness and moderation are key to navigating this delicate relationship between indulgence and intolerance.
Hannaford Brand Sprinkle Cheese: My Honest Review and Usage Tips
You may want to see also

Saturated Fat Concerns: Cheese's saturated fat content can stimulate stomach acid secretion, potentially causing discomfort
Cheese, a beloved staple in many diets, often raises concerns due to its high saturated fat content. This fat, while contributing to its rich flavor and creamy texture, can have a less desirable effect on the digestive system. Saturated fats are known to stimulate the secretion of stomach acid, a process that, in excess, can lead to discomfort for some individuals. Understanding this relationship is crucial for those who enjoy cheese but experience gastrointestinal issues.
From an analytical perspective, the mechanism behind this discomfort lies in the body’s response to saturated fats. When consumed, these fats trigger the release of gastrin, a hormone that increases stomach acid production. For most people, this process is manageable, but for those with sensitive stomachs or conditions like gastroesophageal reflux disease (GERD), the heightened acid levels can exacerbate symptoms. Studies suggest that reducing saturated fat intake, including from cheese, may alleviate acid-related discomfort. For instance, limiting daily saturated fat consumption to less than 10% of total calories, as recommended by dietary guidelines, can help mitigate these effects.
Practically speaking, managing cheese intake requires awareness and moderation. For adults, a serving size of cheese (about 1.5 ounces) contains approximately 5–6 grams of saturated fat, depending on the type. Hard cheeses like cheddar or Parmesan tend to have higher saturated fat content compared to softer varieties like mozzarella or feta. To minimize discomfort, consider pairing cheese with foods that neutralize stomach acid, such as vegetables or whole grains. Additionally, spacing out cheese consumption throughout the day rather than eating large amounts at once can reduce the immediate burden on the digestive system.
A comparative approach reveals that not all cheeses are created equal in terms of their impact on stomach acid. For example, goat cheese, with its lower lactose and fat content, may be a better option for those prone to acid-related issues. Similarly, opting for low-fat or part-skim versions of favorite cheeses can significantly reduce saturated fat intake without sacrificing flavor entirely. Experimenting with different types and observing individual tolerance levels can help identify which cheeses are less likely to cause discomfort.
In conclusion, while cheese’s saturated fat content can stimulate stomach acid secretion, practical adjustments can make it possible to enjoy this food without adverse effects. By understanding the science, monitoring portion sizes, and choosing wiser options, individuals can balance their love for cheese with digestive comfort. As with any dietary concern, listening to one’s body and making informed choices is key to maintaining a healthy relationship with this dairy delight.
Making Farmers Cheese: Milk-to-Cheese Yield from 1 Gallon Explained
You may want to see also
Explore related products

Fermented Cheese Effects: Aged cheeses may reduce acid issues due to lower lactose and easier digestion
Aged cheeses, such as cheddar, Parmesan, and Gouda, undergo a fermentation process that significantly reduces their lactose content. This is crucial for individuals with lactose intolerance, as lactose is the sugar in milk that often triggers digestive discomfort. During aging, bacteria break down lactose into lactic acid, leaving behind a product that is easier on the stomach. For example, a 30-gram serving of aged cheddar contains less than 0.5 grams of lactose, compared to 3 grams in the same amount of fresh cheese like mozzarella. This reduction can minimize acid reflux and other gastrointestinal issues associated with lactose malabsorption.
The fermentation process not only lowers lactose but also enhances the digestibility of aged cheeses. As cheese ages, its protein structure changes, becoming more broken down and easier for the body to process. This is particularly beneficial for those who experience acid-related discomfort after consuming dairy. For instance, pairing a small portion of aged cheese (around 20–30 grams) with a meal can act as a buffer against stomach acid, reducing the likelihood of heartburn. However, moderation is key, as excessive consumption can still lead to acidity due to the cheese’s high fat content.
Practical tips for incorporating aged cheeses into a low-acid diet include choosing varieties aged for at least six months, as these have the lowest lactose levels. Opt for harder cheeses like Gruyère or Pecorino, which are naturally lower in lactose and easier to digest. Pairing aged cheese with alkaline foods, such as leafy greens or nuts, can further mitigate acid issues. For those monitoring portion sizes, a serving equivalent to two dice-sized cubes is sufficient to enjoy the benefits without overindulging.
Comparatively, while fresh cheeses like ricotta or cottage cheese can exacerbate acid problems due to their higher lactose content, aged cheeses offer a viable alternative for cheese lovers. Studies suggest that individuals with mild lactose intolerance can tolerate up to 12 grams of lactose per sitting, making a 30-gram portion of aged cheese well within safe limits. This makes aged cheeses a smart choice for those seeking to reduce acid-related discomfort without eliminating cheese entirely from their diet.
In conclusion, aged cheeses provide a unique solution for managing acid issues through their reduced lactose content and improved digestibility. By selecting the right types and portions, individuals can enjoy cheese without the usual drawbacks. For best results, combine aged cheese with a balanced diet and mindful eating habits, ensuring that this fermented delight remains a friend, not a foe, to your digestive system.
Tyramine Levels in Mozzarella Cheese: What You Need to Know
You may want to see also

Portion Control Tips: Limiting cheese intake and pairing with alkaline foods can minimize acid-related problems
Cheese, a beloved staple in many diets, can tip the scales toward acidity when consumed in excess. Its high fat and protein content, coupled with low pH levels, makes it a potent contributor to acid reflux, heartburn, and other acid-related issues. For individuals prone to these conditions, understanding how to manage cheese intake is crucial. Portion control isn’t about deprivation; it’s about mindful consumption to maintain balance. A single serving of cheese—about 1.5 ounces, or the size of your thumb—is a reasonable daily limit for most people. Exceeding this can overwhelm the body’s acid-neutralizing mechanisms, particularly in those with sensitive digestive systems.
Pairing cheese with alkaline foods is a strategic way to offset its acidity. Alkaline foods, such as leafy greens, cucumbers, and avocados, have a pH-balancing effect that can mitigate the acid load from cheese. For instance, topping a small portion of cheese with a generous serving of spinach or pairing it with a side of sliced cucumber can create a more neutral meal. This approach doesn’t eliminate cheese’s acidity but dilutes its impact, making it easier for the body to manage. For those with chronic acid issues, this pairing method can be a game-changer, allowing them to enjoy cheese without discomfort.
Practical tips for portion control include using measuring tools to avoid overeating and incorporating cheese as a flavor enhancer rather than the main component of a meal. For example, instead of a heavy macaroni and cheese dish, opt for a sprinkle of grated cheddar over a vegetable-rich stir-fry. Another strategy is to choose lower-fat cheese options, as reduced fat content often correlates with lower acidity. However, be cautious of processed low-fat cheeses, which may contain additives that exacerbate acid-related problems. Fresh, natural cheeses like mozzarella or feta are better choices.
Age and health status play a role in how cheese affects acidity. Older adults, whose digestive systems may produce less acid-neutralizing stomach acid, are more susceptible to acid-related issues from cheese. Similarly, individuals with conditions like gastroesophageal reflux disease (GERD) need to be particularly vigilant. For these groups, limiting cheese to 1–2 servings per week and always pairing it with alkaline foods can be a safer approach. Consulting a healthcare provider or dietitian for personalized advice is always recommended.
In conclusion, managing cheese intake through portion control and strategic food pairing can significantly reduce acid-related problems. By focusing on moderation and balance, cheese lovers can continue to enjoy this dairy delight without compromising their digestive health. Small, mindful adjustments—like measuring portions, choosing the right types of cheese, and incorporating alkaline foods—can make a substantial difference. It’s not about eliminating cheese but about eating it smarter.
Shredded Cheese Measurements: How Much is 30g in Volume?
You may want to see also
Frequently asked questions
Yes, consuming too much cheese can worsen acid reflux because it is high in fat, which relaxes the lower esophageal sphincter (LES), allowing stomach acid to flow back into the esophagus.
Yes, excessive cheese intake can lead to stomach acid issues due to its high fat and protein content, which slows digestion and increases the risk of acid production and discomfort.
Yes, too much cheese can aggravate GERD (gastroesophageal reflux disease) as it is acidic and fatty, both of which can trigger symptoms like heartburn and indigestion.