The peculiar phenomenon of cheese under toenail refers to the accumulation of a foul-smelling, yellowish or whitish substance beneath the toenail, often accompanied by discomfort or pain. This condition, medically known as onycholysis or keratin debris, can result from various factors such as fungal infections, poor foot hygiene, trauma, or underlying health issues. The term cheese is used colloquially to describe the soft, crumbly texture and odor reminiscent of certain dairy products, though it is essential to clarify that this substance is not related to actual cheese. Understanding the causes, symptoms, and treatment options for this condition is crucial for maintaining proper foot health and preventing potential complications.
Explore related products
What You'll Learn

Causes of Cheese Under Toenail
The term "cheese under toenail" is a colloquial description for a buildup of debris, often a mix of dead skin, dirt, and sometimes fungal growth, that accumulates beneath the toenail. This unsightly and sometimes odorous condition can be both a cosmetic concern and a potential health issue. Understanding its causes is the first step toward prevention and treatment.
Fungal Infections: The Primary Culprit
The most common cause of cheese-like debris under the toenail is a fungal infection, medically known as onychomycosis. Fungi thrive in warm, moist environments, making toenails particularly susceptible due to their confinement in shoes and socks. When fungi invade the nail bed, they break down the keratin in the nail, leading to discoloration, thickening, and the accumulation of crumbly, yellowish debris. This debris often resembles cheese in texture and appearance. Risk factors include walking barefoot in public areas like pools or gyms, poor foot hygiene, and a weakened immune system. Treatment typically involves antifungal medications, such as topical creams (e.g., terbinafine) or oral prescriptions (e.g., itraconazole), but consistency is key—treatment can last 6–12 months for full recovery.
Poor Foot Hygiene: A Preventable Contributor
Neglecting proper foot care creates an ideal environment for debris buildup. Failing to wash feet regularly, not drying them thoroughly after bathing, or wearing the same socks for multiple days can trap moisture and dead skin cells under the nails. Over time, this accumulation hardens and takes on a cheese-like consistency. Simple preventive measures include washing feet daily with soap, drying them completely (especially between toes), and changing socks frequently. For those prone to sweating, using antifungal foot powder can help keep moisture at bay.
Trauma and Nail Damage: A Hidden Trigger
Physical injury to the toenail, such as stubbing your toe or wearing ill-fitting shoes, can create small gaps between the nail and nail bed. These gaps allow dirt and debris to become trapped, leading to buildup. Repeated trauma can also weaken the nail structure, making it more susceptible to fungal infections. To minimize risk, opt for shoes that provide ample toe room and avoid activities that put excessive pressure on the toes. If injury occurs, keep the area clean and monitor for signs of infection.
Underlying Health Conditions: The Overlooked Factor
Certain health conditions can predispose individuals to toenail debris. Diabetes, for instance, reduces blood flow to the feet and weakens the immune system, making it harder to fight off infections. Psoriasis, a skin condition, can also affect nails, causing them to thicken and accumulate debris. Poor circulation, often linked to peripheral artery disease, slows healing and increases the likelihood of nail issues. If you have an underlying condition, regular foot exams and proactive care are essential. Consult a healthcare provider for tailored advice, such as daily foot inspections for diabetics or moisturizers to manage psoriasis-related dryness.
By addressing these causes—whether through antifungal treatment, improved hygiene, injury prevention, or managing health conditions—you can effectively combat the issue of cheese under the toenail. Early intervention not only restores nail appearance but also prevents complications like severe infection or permanent nail damage.
McDonald's Cheese Change: Fact or Fiction? Uncovering the Truth
You may want to see also

Symptoms and Identification Tips
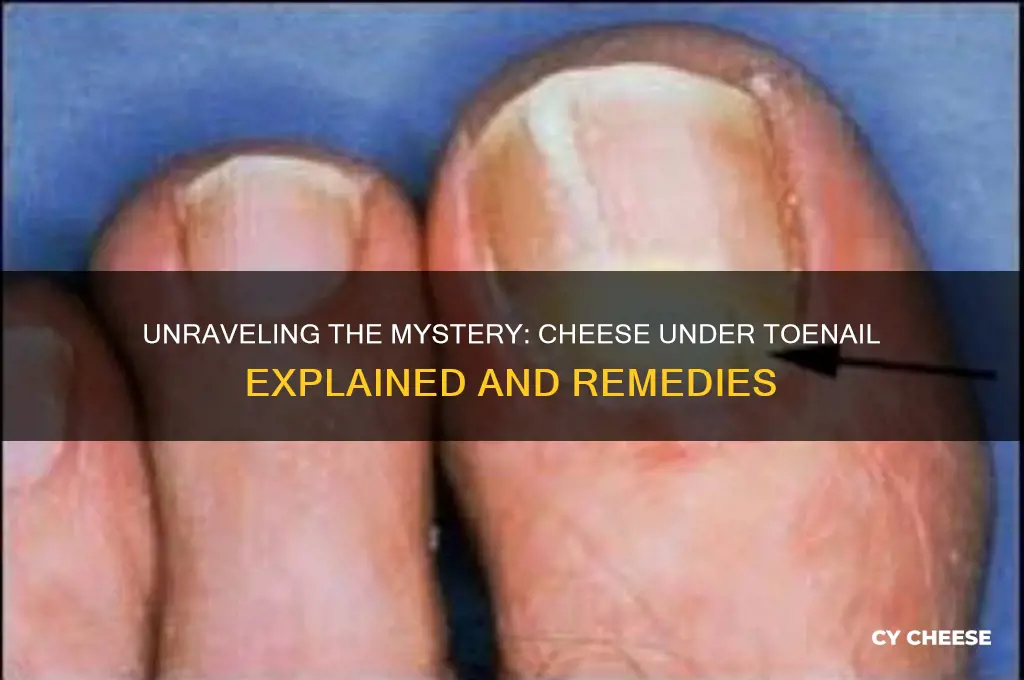
The presence of a cheesy substance under a toenail often indicates a fungal infection, specifically onychomycosis. This condition thrives in warm, moist environments, making toenails particularly susceptible due to their confinement in shoes. The "cheese" is actually debris composed of keratin (a protein in nails), skin cells, and fungal material. It accumulates as the fungus degrades the nail, creating a yellowish, crumbly texture that resembles soft cheese. This debris often emits a foul odor, another telltale sign of infection.
Identifying this issue requires careful observation. Start by examining the nail’s appearance. Early stages may show slight discoloration (white or yellow spots) and thickening. As the infection progresses, the nail may become brittle, ragged, or distorted, with visible crumbling edges. The cheesy debris typically collects under the nail’s free edge or in pockets where the nail lifts from the nail bed. If you gently scrape the nail’s surface with a sterile tool, the powdery or granular residue confirms the presence of fungal debris.
To differentiate this from other conditions, consider the context. Psoriasis or eczema may cause similar nail changes but lack the cheesy debris and odor. Trauma or injury might lead to nail thickening but won’t produce the characteristic fungal breakdown. If you’re unsure, a dermatologist can perform a potassium hydroxide (KOH) test, where a sample of the debris is examined under a microscope to identify fungal elements. Early identification is crucial, as untreated onychomycosis can spread to other nails or cause permanent damage.
Practical tips for self-assessment include maintaining good lighting during inspection and using a magnifying glass if needed. Keep nails trimmed and clean to prevent debris buildup, which can worsen the infection. Avoid picking or digging at the nail, as this can introduce bacteria and lead to secondary infections. If you notice persistent changes or discomfort, consult a healthcare professional for proper diagnosis and treatment options, such as topical antifungals or oral medications.
String Cheese and Potassium: Unraveling the Nutritional Facts
You may want to see also

Effective Home Remedies
The buildup of keratin debris under toenails, often mistaken for cheese due to its appearance, can be addressed with targeted home remedies. One effective approach is the use of urea-based creams, which break down the hardened protein. Apply a 40% urea cream nightly, covering the area with a bandage to enhance absorption. This method is particularly beneficial for adults over 50, as keratin buildup tends to worsen with age. Consistency is key—results may take 2–4 weeks, but the gradual softening of debris prevents aggressive scraping, reducing injury risk.
For those seeking a natural alternative, a warm vinegar soak can dissolve keratin and restore nail clarity. Mix equal parts white vinegar and warm water, soaking the affected foot for 20 minutes daily. Vinegar’s acetic acid softens the debris, while its antimicrobial properties curb bacterial growth. This remedy is safe for all ages but may cause mild stinging in individuals with sensitive skin. Pairing the soak with a gentle nail brush can expedite results, but avoid vigorous scrubbing to prevent irritation.
Tea tree oil, renowned for its antifungal and antiseptic qualities, offers another potent solution. Dilute 2–3 drops of tea tree oil in a teaspoon of coconut oil and apply directly to the toenail twice daily. The oil’s terpinen-4-ol compound penetrates the nail bed, breaking down keratin while inhibiting fungal infections. This remedy is ideal for individuals prone to athlete’s foot or toenail fungus. However, patch test first to ensure no allergic reaction occurs, especially in children or those with eczema.
Comparing these methods, urea creams provide the most consistent results for severe buildup but require patience. Vinegar soaks are gentler and more immediate but may not address deeply embedded debris. Tea tree oil is best for those with concurrent fungal concerns, though its potency demands careful application. Each remedy’s efficacy depends on the severity of the condition and the user’s commitment to daily maintenance. Combining approaches—such as a vinegar soak followed by urea cream—can yield faster, more comprehensive results.
Finally, prevention plays a critical role in managing keratin buildup. Trim toenails straight across, avoiding tight footwear that compresses toes, and maintain proper foot hygiene. For diabetics or those with poor circulation, consult a podiatrist before attempting home treatments. While these remedies effectively address "cheese" under toenails, persistent or painful symptoms warrant professional evaluation to rule out underlying conditions like psoriasis or onychomycosis.
Caesar's Rotisserie Chicken: Bacon, Cheese, and Culinary Delight
You may want to see also
Explore related products

When to See a Doctor
If you notice a yellowish or whitish substance resembling cheese under your toenail, it’s likely a fungal infection known as onychomycosis. While mild cases may not require immediate medical attention, certain signs indicate it’s time to see a doctor. Persistent pain, swelling, or redness around the nail suggests the infection has deepened, potentially affecting the nail bed or surrounding skin. Ignoring these symptoms can lead to complications, such as cellulitis, especially in individuals with diabetes or weakened immune systems. Early intervention is key to preventing further damage and ensuring effective treatment.
For those unsure whether their condition warrants medical attention, consider this rule of thumb: if over-the-counter antifungal creams or topical solutions show no improvement after 4–6 weeks, consult a healthcare professional. A doctor can perform a nail clipping or scraping to confirm the presence of fungus and determine its type. This is crucial because different fungi may require specific treatments, such as oral antifungal medications like terbinafine or itraconazole. Note that oral treatments often require a 6–12 week course and may interact with other medications, so a doctor’s oversight is essential.
Children and older adults should seek medical advice sooner rather than later. Children’s nails grow faster, and early treatment can prevent the infection from spreading to other nails. Older adults, particularly those with poor circulation or diabetes, are at higher risk of complications. For instance, a seemingly minor toenail fungus can lead to ulcers or infections that are harder to treat in these populations. A podiatrist or dermatologist can provide tailored solutions, such as debridement (removal of infected nail material) or laser therapy, which may be more suitable for specific age groups.
Lastly, if you experience systemic symptoms like fever, chills, or drainage from the nail, seek immediate medical attention. These signs could indicate a secondary bacterial infection, which requires urgent treatment, often with oral antibiotics. Even if you’re tempted to self-treat, remember that some home remedies, like vinegar soaks or tea tree oil, lack scientific backing for severe cases. A doctor can offer evidence-based options and monitor your progress to ensure the infection is fully resolved, reducing the risk of recurrence.
Who Invited Cheese? Unraveling the Mystery Behind Its Global Popularity
You may want to see also

Prevention and Foot Hygiene
The accumulation of debris under toenails, often likened to the texture and color of cheese, is a common yet preventable issue. This buildup, typically a mix of dead skin, dirt, and moisture, thrives in the warm, dark environment of shoes. Regular foot hygiene is the cornerstone of prevention, starting with daily washing using mild soap and warm water. Ensure thorough drying, especially between toes, as residual moisture fosters bacterial and fungal growth. Trim toenails straight across to discourage debris accumulation and reduce the risk of ingrown nails, a frequent contributor to under-nail buildup.
Instructive in nature, the integration of antifungal foot powders or sprays into daily routines can significantly mitigate risks. Apply these products to both feet and the interior of shoes, particularly if prone to sweating. For individuals with hyperhidrosis, consider moisture-wicking socks and rotate shoes daily to allow them to dry completely. Avoid walking barefoot in communal areas like pools or locker rooms, where fungal infections often spread. Instead, wear waterproof sandals or flip-flops to create a barrier against contaminants.
Persuasively, investing in proper footwear is not just about style but also about foot health. Shoes should fit well, allowing adequate airflow and providing proper support. Tight or ill-fitting shoes compress toes, increasing friction and the likelihood of debris accumulation. For those with active lifestyles, prioritize breathable materials like leather or mesh, and replace athletic shoes every 6–12 months, depending on usage. Custom orthotics can also improve foot mechanics, reducing pressure points that contribute to under-nail issues.
Comparatively, while over-the-counter remedies like urea-based creams or salicylic acid treatments can manage mild cases, persistent or severe buildup warrants professional intervention. Podiatrists may perform debridement to remove hardened debris or prescribe topical antifungal medications. For systemic infections, oral antifungals such as terbinafine (250 mg daily for 6–12 weeks) may be necessary, though these require monitoring for potential side effects like liver toxicity. Early consultation prevents complications like nail detachment or secondary bacterial infections.
Descriptively, maintaining foot hygiene extends beyond the nails to overall skin health. Exfoliate feet weekly with a pumice stone or foot file to remove dead skin, but avoid aggressive scrubbing that can cause micro-tears. Moisturize daily with emollient-rich creams, steering clear of the areas between toes to prevent excess moisture buildup. Incorporate a foot soak with Epsom salt (1/2 cup per gallon of warm water) for 15–20 minutes to reduce inflammation and soften skin. These practices not only prevent "cheese" under toenails but also promote overall foot comfort and appearance.
Is Colby Jack Real Cheese? Unraveling the Mystery Behind the Blend
You may want to see also
Frequently asked questions
The term "cheese" under toenail often refers to a buildup of debris, dead skin, or fungal material that resembles cheese in texture or appearance. It can indicate a fungal infection, poor hygiene, or an ingrown toenail.
To remove the buildup, gently clean the area with warm, soapy water and a soft brush. If it’s due to a fungal infection, antifungal treatments or medications may be necessary. Consult a podiatrist for persistent or severe cases.
Yes, cheese-like material under the toenail can be a sign of a fungal infection, such as toenail fungus (onychomycosis). It may also indicate bacterial growth or other underlying issues, especially if accompanied by pain, redness, or swelling.











































