When cheese irritates your stomach, it is often referred to as lactose intolerance or dairy sensitivity. This occurs because many people lack sufficient lactase, the enzyme needed to break down lactose, a sugar found in milk and dairy products like cheese. As a result, undigested lactose ferments in the gut, leading to symptoms such as bloating, gas, abdominal pain, and diarrhea. For some individuals, the issue may also be related to casein, a milk protein, which can trigger discomfort in those with sensitivities or conditions like irritable bowel syndrome (IBS). Understanding the cause of this irritation is key to managing symptoms and making informed dietary choices.
Explore related products
What You'll Learn

Lactose Intolerance Symptoms
Cheese, a beloved staple in many diets, can turn from friend to foe for those with lactose intolerance. This condition occurs when the body lacks sufficient lactase, the enzyme needed to break down lactose, a sugar found in milk and dairy products. The resulting symptoms can range from mildly uncomfortable to severely disruptive, often leaving individuals wondering why their favorite foods suddenly cause distress.
Symptoms and Their Onset
Identifying the Culprit
Not all dairy products affect individuals equally. Cheese, for example, varies in lactose content. Hard cheeses like cheddar or Swiss have lower lactose levels due to the fermentation process, making them more tolerable for some. Conversely, soft or processed cheeses retain more lactose, increasing the likelihood of irritation. Keeping a food diary can help pinpoint which types of cheese trigger symptoms, allowing for better dietary management.
Managing Symptoms Effectively
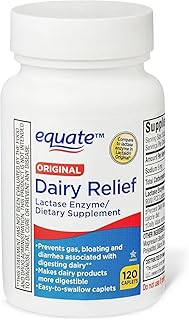
For those who love cheese but struggle with lactose intolerance, moderation and strategic choices are key. Opting for lactose-free or reduced-lactose cheese varieties can provide a satisfying alternative. Pairing cheese with other foods can also slow digestion, reducing the risk of symptoms. Over-the-counter lactase enzymes, taken before meals, can help break down lactose, though effectiveness varies by individual. Consulting a healthcare provider for personalized advice is always recommended, especially if symptoms persist or worsen.
Long-Term Considerations
While lactose intolerance is not life-threatening, its symptoms can significantly impact quality of life. Chronic discomfort may lead to avoidance of social situations involving food or nutritional deficiencies if dairy is a primary calcium source. Incorporating non-dairy calcium sources like leafy greens, fortified plant milks, or supplements can help maintain bone health. Understanding and adapting to lactose intolerance allows individuals to enjoy cheese and other foods without sacrificing well-being.
Exploring the Farms Behind Oscar Mayer's Cheese Production
You may want to see also

Dairy Sensitivity Causes
Experiencing stomach irritation after consuming cheese often points to dairy sensitivity, a condition where the body struggles to process lactose or reacts to other components in dairy products. This discomfort can manifest as bloating, gas, diarrhea, or abdominal pain, leaving many to wonder why cheese, a beloved staple in diets worldwide, can be so troublesome. Understanding the root causes of dairy sensitivity is crucial for managing symptoms and making informed dietary choices.
One primary cause of dairy sensitivity is lactose intolerance, a condition where the body lacks sufficient lactase, the enzyme needed to break down lactose, the sugar found in milk and dairy products. When lactose remains undigested, it ferments in the gut, producing gas and drawing water into the intestines, leading to the familiar symptoms of discomfort. Interestingly, lactose intolerance is more common in certain populations, such as those of East Asian, West African, Arab, Jewish, Greek, and Italian descent, where up to 90% of adults may be affected. Age also plays a role, as lactase production naturally declines after infancy, making lactose intolerance more prevalent in adulthood.
Another lesser-known cause of dairy sensitivity is an intolerance to milk proteins, specifically casein and whey. Unlike lactose intolerance, this reaction involves the immune system, which mistakenly identifies these proteins as harmful, triggering inflammation and digestive symptoms. This type of sensitivity is often confused with a milk allergy, but it lacks the severe, systemic allergic response. Individuals with this condition may find that even small amounts of cheese or other dairy products provoke symptoms, making it essential to identify and eliminate these triggers.
Emerging research also suggests that dairy sensitivity could be linked to the gut microbiome. An imbalance in gut bacteria can impair digestion and increase susceptibility to food sensitivities. For instance, a diet high in processed foods and low in fiber can disrupt microbial diversity, potentially exacerbating reactions to dairy. Probiotics and prebiotics may offer relief by restoring gut health, though more studies are needed to establish clear guidelines.
Practical steps to manage dairy sensitivity include gradually reducing dairy intake to assess tolerance levels, opting for lactose-free or low-lactose products, and exploring alternatives like almond, oat, or coconut-based cheeses. Keeping a food diary can help pinpoint specific triggers, while consulting a healthcare provider or dietitian ensures a tailored approach. For those with protein sensitivities, reading labels carefully to avoid hidden dairy ingredients is crucial. By understanding the causes and taking proactive measures, individuals can enjoy a balanced diet without the discomfort cheese often brings.
Cheese Snake Strategically: Smouldering Lake Ballista's Best Spots Revealed
You may want to see also

Cheese and Digestive Issues
Cheese, a beloved staple in many diets, can sometimes turn from friend to foe for your digestive system. The culprit often lies in its lactose content, a sugar found in milk and dairy products. When the body lacks sufficient lactase, the enzyme needed to break down lactose, it can lead to discomfort. This condition, known as lactose intolerance, affects a significant portion of the global population, particularly as people age. Symptoms such as bloating, gas, abdominal pain, and diarrhea typically emerge 30 minutes to two hours after consuming dairy products like cheese. Understanding this connection is the first step in managing digestive issues related to cheese.
Not all cheeses are created equal when it comes to lactose content. Hard cheeses like cheddar, Parmesan, and Swiss undergo a longer aging process, which naturally reduces their lactose levels. These varieties are often better tolerated by individuals with lactose intolerance. On the other hand, soft cheeses like ricotta, cream cheese, and fresh mozzarella retain higher lactose levels, making them more likely to irritate sensitive stomachs. For those experimenting with cheese consumption, starting with small portions of hard cheeses and monitoring reactions can be a practical approach. Keeping a food diary to track symptoms and specific cheeses consumed can also help identify patterns.
Beyond lactose, another potential irritant in cheese is its high fat content. Fatty foods, in general, can slow down digestion and exacerbate conditions like gastroesophageal reflux disease (GERD) or irritable bowel syndrome (IBS). Blue cheeses, for instance, are not only high in fat but also contain histamine, a compound that can trigger digestive discomfort in some individuals. For those with fat sensitivity, opting for low-fat cheese varieties or consuming cheese in moderation may alleviate symptoms. Pairing cheese with fiber-rich foods like whole-grain crackers or vegetables can also aid digestion by balancing the meal’s macronutrient profile.
For individuals determined to enjoy cheese without the aftermath, exploring alternatives and remedies can be beneficial. Lactase enzyme supplements, available over the counter, can be taken before consuming dairy to help break down lactose. Additionally, fermented dairy products like aged cheeses or lactose-free cheese options are increasingly available in markets. Probiotic-rich foods, such as yogurt or kefir, can also support gut health and improve tolerance to dairy over time. Consulting a healthcare provider or dietitian for personalized advice is always a wise step, especially for those with chronic digestive conditions. With the right strategies, cheese can remain a delightful part of the diet without causing undue discomfort.
Is the Moon Made of Cheese? Exploring a Widespread Myth
You may want to see also
Explore related products
$8.69 $10.22

Fermentable Oligosaccharides Impact
Cheese, a beloved staple in many diets, can sometimes turn from friend to foe, leaving your stomach in distress. This discomfort often stems from Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols (FODMAPs), a group of carbohydrates found in various foods, including certain types of cheese. Understanding the impact of these fermentable oligosaccharides is crucial for anyone who experiences gastrointestinal irritation after indulging in cheesy delights.
The Science Behind the Discomfort
Fermentable oligosaccharides, such as galactans and fructans, are present in aged cheeses like cheddar, gouda, and blue cheese. These compounds resist digestion in the small intestine, traveling instead to the large intestine where they are fermented by gut bacteria. This fermentation process produces gas, leading to bloating, cramps, and even diarrhea—symptoms commonly associated with irritable bowel syndrome (IBS). For individuals with lactose intolerance, the combination of lactose (a disaccharide) and oligosaccharides in cheese can exacerbate stomach irritation, creating a double-whammy effect.
Practical Tips for Cheese Lovers
If you suspect fermentable oligosaccharides are the culprits behind your cheese-induced discomfort, consider these actionable steps. First, opt for low-FODMAP cheeses like feta, mozzarella, or cream cheese, which contain minimal oligosaccharides. Second, monitor portion sizes; even low-FODMAP cheeses can trigger symptoms if consumed in excess. For example, a serving of 40 grams (about 1.4 ounces) of feta is generally well-tolerated. Pairing cheese with digestive enzymes, such as lactase supplements, can also help break down lactose and reduce irritation.
Comparing High and Low-FODMAP Cheeses
Not all cheeses are created equal when it comes to fermentable oligosaccharides. Hard, aged cheeses like parmesan and pecorino are higher in these compounds due to their prolonged fermentation processes. In contrast, fresh cheeses like ricotta and cottage cheese have lower FODMAP levels, making them gentler on the stomach. A comparative analysis reveals that a 30-gram serving of cheddar (high-FODMAP) can produce significantly more gas than the same amount of brie (moderate-FODMAP) or cream cheese (low-FODMAP). This highlights the importance of choosing cheese wisely based on individual tolerance.
Long-Term Strategies for Gut Health
While avoiding high-FODMAP cheeses is a quick fix, addressing the root cause of sensitivity to fermentable oligosaccharides can provide lasting relief. Incorporating gut-friendly foods like probiotics (yogurt, kefir) and prebiotics (bananas, oats) can strengthen the gut microbiome, improving tolerance to FODMAPs over time. For those with severe reactions, consulting a dietitian to develop a personalized low-FODMAP diet plan is advisable. This structured approach involves eliminating high-FODMAP foods for 2–6 weeks, then gradually reintroducing them to identify specific triggers.
In summary, fermentable oligosaccharides in cheese can irritate the stomach, but with knowledge and strategic choices, cheese lovers can still enjoy their favorite dairy without discomfort. By selecting low-FODMAP options, monitoring portions, and supporting gut health, the impact of these compounds can be minimized, ensuring a harmonious relationship between cheese and your digestive system.
Should You Change the Water for Fresh Mozzarella Cheese?
You may want to see also

Histamine Intolerance Effects
Cheese, a beloved staple in many diets, can sometimes turn from friend to foe, leaving you with an upset stomach. This discomfort often stems from histamine intolerance, a condition where the body struggles to break down histamine, a compound naturally present in aged cheeses, fermented foods, and certain beverages. Unlike a typical food allergy, histamine intolerance triggers a cascade of symptoms that mimic an allergic reaction but are rooted in metabolic dysfunction. Understanding its effects is crucial for anyone who’s ever wondered why their favorite cheddar or brie leaves them feeling unwell.
Histamine intolerance manifests through a range of symptoms, often mistaken for other conditions. Common effects include gastrointestinal distress—such as bloating, cramps, and diarrhea—shortly after consuming histamine-rich foods like aged cheeses. But it doesn’t stop there. Headaches, migraines, skin rashes, and even heart palpitations can occur, as histamine dilates blood vessels and stimulates nerve endings. For instance, a single serving of Parmesan, which contains up to 400 mg of histamine per 100 grams, can trigger symptoms in sensitive individuals. Recognizing these patterns is the first step in identifying whether histamine intolerance is the culprit behind your cheese-induced discomfort.
Managing histamine intolerance involves more than just avoiding cheese. It requires a strategic approach to diet and lifestyle. Start by keeping a food diary to track symptoms and identify high-histamine culprits. Opt for fresh, unprocessed foods and limit fermented or aged products. For example, swap aged cheddar for fresh mozzarella, which contains significantly less histamine. Additionally, certain medications, like antihistamines or DAO enzyme supplements (dosage: 200–400 HDU before meals), can help alleviate symptoms. However, consult a healthcare provider before starting any new regimen, especially if you’re pregnant, nursing, or over 65, as individual needs vary.
One often-overlooked aspect of histamine intolerance is its interplay with gut health. A compromised gut microbiome can exacerbate symptoms, as beneficial bacteria play a role in histamine metabolism. Incorporating low-histamine probiotics, such as *Lactobacillus rhamnosus*, and prebiotic-rich foods like bananas or oats can support gut repair. Conversely, alcohol and stress, which increase histamine release, should be minimized. For instance, pairing a low-histamine meal with a glass of wine could undo your efforts, as alcohol blocks DAO enzyme activity, the body’s primary histamine-degrading mechanism.
Finally, while histamine intolerance can feel restrictive, it’s manageable with awareness and planning. Experiment with low-histamine recipes, like fresh vegetable stir-fries or herb-infused olive oil dips, to enjoy flavorful meals without discomfort. Remember, the goal isn’t to eliminate cheese entirely but to understand your threshold and make informed choices. By addressing histamine intolerance head-on, you can reclaim your love for food while keeping your stomach happy.
McDonald's Quarter Pounder with Cheese: Ingredients and Toppings Revealed
You may want to see also
Frequently asked questions
It is often referred to as lactose intolerance or dairy sensitivity, as cheese contains lactose, a sugar that some people have difficulty digesting.
Cheese contains lactose, and if your body lacks the enzyme lactase to break it down, it can cause digestive issues like bloating, gas, and stomach pain.
Yes, some people may still experience discomfort due to other components in cheese, such as milk proteins (casein or whey) or its high fat content.
You can try lactose-free cheese, take lactase enzyme supplements before eating cheese, or opt for fermented cheeses like cheddar or Swiss, which have lower lactose levels.