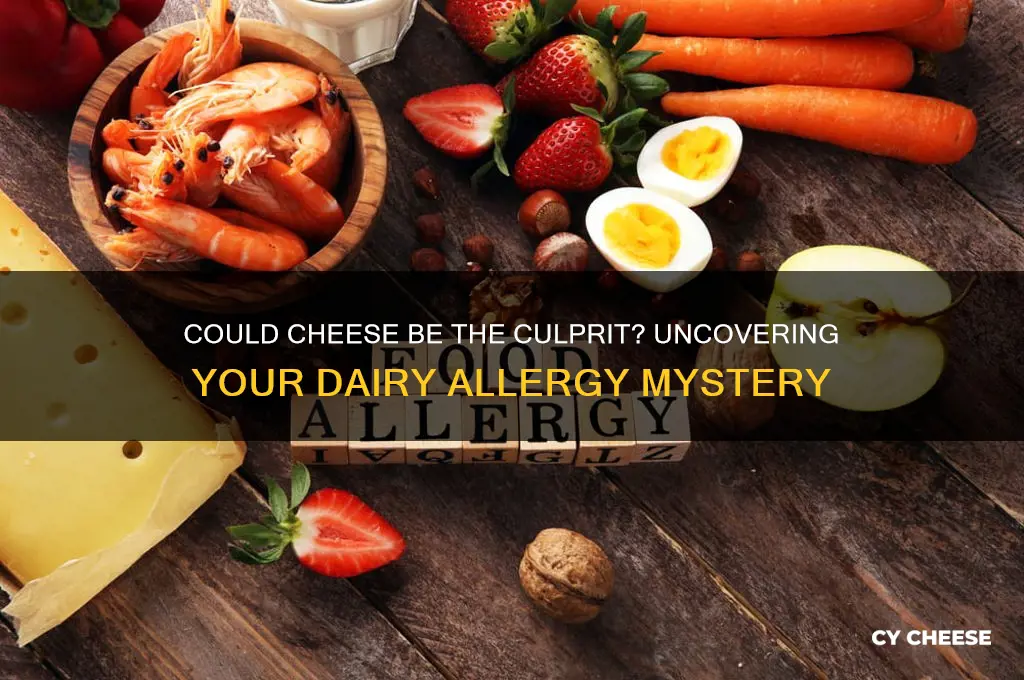
If you’re wondering, Am I allergic to cheese? you’re not alone—many people experience discomfort after consuming dairy products, but it’s important to distinguish between a true allergy and other conditions like lactose intolerance or sensitivity. A cheese allergy is rare and typically involves an immune response to proteins found in milk, such as casein or whey, which can cause symptoms like hives, swelling, digestive issues, or even anaphylaxis in severe cases. However, lactose intolerance, which is more common, results from the body’s inability to digest lactose, a sugar in milk, leading to bloating, gas, or diarrhea. To determine if you’re allergic to cheese, consult an allergist for testing, as self-diagnosis can be misleading. Understanding the root cause of your symptoms is crucial for managing your diet and overall health effectively.
| Characteristics | Values |
|---|---|
| Symptoms | Itching, swelling, hives, digestive issues (nausea, vomiting, diarrhea), respiratory problems, anaphylaxis (rare) |
| Cause | Allergy to milk proteins (casein or whey), lactose intolerance (not an allergy but often confused), histamine intolerance |
| Prevalence | Rare (true cheese allergy); lactose intolerance is more common |
| Diagnosis | Skin prick test, blood test (IgE antibodies), oral food challenge, elimination diet |
| Treatment | Avoidance of cheese and dairy products, antihistamines for mild reactions, epinephrine for severe reactions (anaphylaxis) |
| Cross-Reactivity | Possible with other dairy products (milk, butter, yogurt), rarely with beef or other foods containing similar proteins |
| Prevention | Read food labels carefully, inform restaurants about allergies, carry emergency medication (if severe) |
| Misconceptions | Not the same as lactose intolerance; symptoms can vary widely in severity |
| Related Conditions | Cow’s milk allergy, lactose intolerance, histamine intolerance |
| Alternative Options | Lactose-free cheese, vegan cheese, fermented dairy products (lower in lactose) |
Explore related products
What You'll Learn

Common Cheese Allergens
Cheese, a beloved staple in many diets, can sometimes be the culprit behind uncomfortable allergic reactions. Understanding the common allergens in cheese is the first step toward identifying whether your symptoms are cheese-related. The primary allergen in cheese is milk protein, specifically casein and whey. These proteins can trigger immune responses in individuals with dairy allergies, leading to symptoms like hives, digestive issues, or even anaphylaxis in severe cases. If you suspect a cheese allergy, it’s crucial to differentiate between a true allergy and lactose intolerance, as the latter involves difficulty digesting milk sugar rather than proteins.
Analyzing the types of cheese can provide insight into potential allergens. Hard cheeses like cheddar or Parmesan contain higher concentrations of casein, making them more likely to cause reactions in sensitive individuals. Conversely, softer cheeses like mozzarella or Brie have lower casein levels but may still pose risks due to added ingredients like molds or preservatives. For example, individuals allergic to mold should avoid blue cheese, as the mold cultures used in its production can trigger allergic responses. Always check labels for additives like annatto (a natural coloring agent) or enzymes, which can also cause adverse reactions in some people.
If you’re testing for a cheese allergy, start with small portions of mild, hard cheeses to gauge your body’s response. Keep a food diary to track symptoms and their severity, noting the type of cheese consumed. For children, who are more prone to dairy allergies, introduce cheese in tiny amounts under supervision and consult a pediatrician if any reactions occur. Adults should monitor symptoms like itching, swelling, or gastrointestinal distress, which typically appear within minutes to hours after consumption. In severe cases, carry an epinephrine auto-injector if prescribed, as cheese allergies can escalate quickly.
Persuasively, it’s worth noting that not all cheese-related discomfort stems from allergies. Lactose intolerance, for instance, causes bloating, gas, and diarrhea due to the body’s inability to digest lactose, not proteins. Similarly, histamine intolerance can mimic allergy symptoms, as aged cheeses like cheddar or Gouda contain high histamine levels that may trigger headaches or skin flushing in sensitive individuals. If you’re unsure, consult an allergist for testing, such as skin prick tests or blood tests, to confirm the root cause of your symptoms.
Practically, managing a cheese allergy involves reading labels meticulously and exploring alternatives. Look for plant-based cheeses made from nuts, soy, or coconut, which are free from dairy proteins. When dining out, ask about ingredients and preparation methods to avoid cross-contamination. For those with mild sensitivities, experimenting with low-histamine or lactose-free cheeses might provide relief. Ultimately, understanding common cheese allergens empowers you to make informed choices, ensuring you can enjoy food safely without compromising your health.
Factors Influencing Milk Curdling in Cheese Making: A Comprehensive Guide
You may want to see also

Symptoms of Cheese Allergy
Cheese, a beloved staple in many diets, can sometimes turn from friend to foe for those with an allergy. Recognizing the symptoms early is crucial for managing discomfort and preventing severe reactions. While cheese allergies are less common than lactose intolerance, they can still cause significant issues for those affected. Symptoms typically manifest within minutes to hours after consumption and can range from mild to severe, depending on the individual’s sensitivity.
One of the most immediate signs of a cheese allergy is digestive distress. This can include abdominal pain, bloating, gas, and diarrhea. These symptoms often arise because the body struggles to process the proteins in cheese, leading to inflammation in the gastrointestinal tract. For children, especially those under five, these symptoms may be more pronounced due to their developing immune systems. If you notice persistent digestive issues after consuming cheese, it’s worth considering an allergy as a potential cause.
Skin reactions are another telltale sign of a cheese allergy. Hives, itching, or eczema can develop shortly after ingestion. In some cases, individuals may experience swelling of the lips, face, or throat, which can be alarming and potentially dangerous. These reactions occur as the immune system releases histamines in response to the allergen. If you develop skin symptoms after eating cheese, avoid further consumption and consult a healthcare professional to determine the cause.
Respiratory symptoms, though less common, can also indicate a cheese allergy. Sneezing, runny nose, coughing, or wheezing may occur as the body tries to expel the allergen. In severe cases, anaphylaxis—a life-threatening reaction characterized by difficulty breathing, rapid heartbeat, and a drop in blood pressure—can occur. Anaphylaxis requires immediate medical attention, and individuals with a history of severe allergies should carry an epinephrine auto-injector (e.g., EpiPen) as a precaution.
To determine if you’re allergic to cheese, start by keeping a food diary to track symptoms after consumption. If you suspect an allergy, consult an allergist for testing, which may include skin prick tests or blood tests to measure IgE antibodies. Eliminating cheese from your diet may be necessary, but it’s essential to do so under professional guidance to ensure nutritional needs are met. Alternatives like lactose-free or vegan cheeses can be explored, but always check labels for potential cross-contamination. Early detection and management are key to living comfortably with a cheese allergy.
Global Cheese Production: Which Country Leads in Annual Output?
You may want to see also

Lactose Intolerance vs. Allergy
If you suspect cheese is causing discomfort, understanding the difference between lactose intolerance and a dairy allergy is crucial. Lactose intolerance occurs when your body lacks lactase, the enzyme needed to digest lactose, a sugar in milk products. Symptoms like bloating, gas, and diarrhea typically appear 30 minutes to 2 hours after consumption. In contrast, a dairy allergy involves your immune system reacting to milk proteins, such as casein or whey, leading to immediate and potentially severe symptoms like hives, swelling, or anaphylaxis.
To distinguish between the two, consider the timing and severity of your reaction. Lactose intolerance symptoms are digestive and gradual, while allergic reactions are rapid and can affect multiple systems. A simple self-test involves monitoring your response to lactose-free dairy products. If symptoms persist, consult a healthcare provider for accurate diagnosis through tests like a hydrogen breath test for lactose intolerance or a skin prick test for allergies.
For those with lactose intolerance, managing symptoms often involves reducing lactose intake rather than eliminating dairy entirely. Hard cheeses like cheddar or Swiss contain minimal lactose, making them better tolerated. Over-the-counter lactase enzymes can also help break down lactose before consumption. Conversely, a dairy allergy requires strict avoidance of all milk proteins, including those in cheese, butter, and even hidden sources like baked goods or processed foods.
Children are more likely to outgrow a milk allergy, with about 80% becoming tolerant by age 16. Lactose intolerance, however, is often a lifelong condition, especially in populations with lower historical dairy consumption, such as those of East Asian or Indigenous American descent. Regardless of age or background, both conditions demand tailored dietary adjustments to maintain health and comfort.
Practical tips include reading labels carefully for hidden dairy in processed foods and exploring alternatives like almond, soy, or oat-based cheeses. For lactose intolerance, gradually reintroduce small amounts of dairy to gauge tolerance, as some individuals can handle up to 12 grams of lactose (about 1 cup of milk) in one sitting. For allergies, carry an epinephrine auto-injector if prescribed, and inform caregivers or dining companions of your condition. Understanding these distinctions empowers you to make informed choices and enjoy a balanced diet without unnecessary restrictions.
Dog Ate Moldy Cheese? Immediate Steps to Ensure Your Pet's Safety
You may want to see also
Explore related products
$16.99 $18.99

Cheese Allergy Testing Options
Suspecting a cheese allergy can be frustrating, especially when symptoms like bloating, rashes, or digestive issues arise after indulging in a favorite dish. Identifying the culprit requires precise testing, as cheese allergies can stem from proteins like casein or whey, or even lactose intolerance masquerading as an allergy. Here’s how to navigate cheese allergy testing options effectively.
Skin Prick Testing: Quick but Not Definitive
A common first step is the skin prick test, where a small amount of cheese extract is applied to the skin after a tiny prick. If a raised bump (wheal) appears within 15–20 minutes, it suggests an allergic reaction. This test is fast, typically performed in an allergist’s office, and suitable for all ages, including children. However, it’s not foolproof. False positives can occur, especially if the skin is irritated or if the extract contains non-allergenic additives. Always follow up with further testing for confirmation.
Blood Tests: Measuring IgE Antibodies
For a less invasive option, blood tests like the ImmunoCAP Specific IgE test measure antibodies produced in response to cheese proteins. A small blood sample is taken, and results are usually available within a week. This method is ideal for those with skin conditions that could interfere with skin prick tests. While it’s highly accurate, it’s also more expensive and may not detect mild allergies. Discuss with your allergist whether this test aligns with your symptoms and medical history.
Elimination Diet: Practical but Time-Consuming
If formal testing isn’t feasible, an elimination diet can provide clarity. Remove all cheese and dairy products from your diet for 2–3 weeks, then reintroduce them one at a time while monitoring symptoms. Keep a detailed food diary to track reactions. This method is cost-effective and doesn’t require medical supervision, but it demands discipline and patience. It’s also less precise, as symptoms may overlap with other intolerances or conditions.
Oral Food Challenge: The Gold Standard
For definitive results, an oral food challenge is the most reliable method. Conducted under medical supervision, you’ll consume small, controlled amounts of cheese in increasing doses while being monitored for reactions. This test can pinpoint specific cheese types or proteins causing issues. However, it’s time-consuming (often 4–6 hours) and carries a risk of severe reactions, so it’s reserved for cases where other tests are inconclusive.
Practical Tips for Testing Success
Regardless of the method chosen, preparation is key. Avoid antihistamines for 3–7 days before skin or blood tests, as they can interfere with results. For oral challenges, ensure you’re in good health and not experiencing any active allergies. Always consult an allergist to determine the most appropriate testing approach based on your symptoms, age, and medical history. With the right strategy, you can finally answer the question: *Am I allergic to cheese?*
Calories in Cheese Slices: A Nutritional Breakdown for Cheese Lovers
You may want to see also

Alternatives to Dairy Cheese
Dairy cheese allergies or intolerances can stem from lactose, casein, or other milk proteins, leaving many searching for satisfying alternatives. Fortunately, the plant-based market has exploded with options that mimic the texture, flavor, and meltability of traditional cheese. Nut-based cheeses, like those made from cashews or almonds, offer a creamy consistency ideal for spreads or dips. For a firmer texture, try coconut oil-based varieties, which excel in grilled cheese sandwiches or cheese boards. Fermented options, such as those made from cultured nuts or seeds, provide probiotic benefits while replicating the tangy depth of aged cheeses.
When selecting dairy-free cheese, consider the intended use. Shredded soy or pea protein-based cheeses melt well for pizzas or casseroles, though they may lack the complexity of dairy cheese. For snacking or charcuterie, opt for aged nut cheeses, which develop sharper, more nuanced flavors over time. Always check labels for additives like carrageenan or excessive oils, which can affect digestion. Experimenting with different brands and types is key, as taste and performance vary widely across products.
Making your own dairy-free cheese at home is simpler than it sounds. Start with a basic cashew cheese recipe: soak 2 cups of raw cashews for 4 hours, blend with ¼ cup nutritional yeast, 2 tablespoons lemon juice, 1 teaspoon garlic powder, and ½ teaspoon salt. Adjust consistency with water or thickness with tapioca starch. For a firmer cheese, press the mixture into a mold, wrap in cheesecloth, and refrigerate for 24 hours. This DIY approach allows customization of flavors and avoids preservatives found in store-bought versions.
For those with nut allergies, seed-based cheeses made from sunflower, pumpkin, or sesame seeds are excellent alternatives. These options are lower in fat and provide a crunchy texture, though they may not melt as smoothly. Another innovative choice is cheese made from legumes, such as chickpeas, which offer a high protein content and a mild, versatile flavor. Pair these alternatives with complementary foods—seed cheeses with crackers, legume-based cheeses in wraps—to enhance their appeal.
Finally, consider the role of dairy-free cheese in a balanced diet. While these alternatives can be healthier, some are high in sodium or saturated fats. Portion control is crucial; a 30g serving (about the size of a matchbox) is a good starting point. Pair dairy-free cheese with fiber-rich foods like vegetables or whole grains to slow digestion and improve satiety. For children or older adults, consult a dietitian to ensure these alternatives meet nutritional needs without overloading on additives. With mindful selection and creativity, dairy-free cheese can be a delicious, inclusive addition to any diet.
Understanding Cheese Block Sizes: How Many Ounces Are in a Block?
You may want to see also
Frequently asked questions
Common symptoms of a cheese allergy include hives, itching, swelling, digestive issues (like nausea or diarrhea), and respiratory problems. If you experience these after consuming cheese, consult a doctor for testing.
Yes, lactose intolerance can cause similar symptoms (bloating, gas, diarrhea) but is not an allergy. An allergy involves the immune system, while lactose intolerance is due to the inability to digest lactose.
Hard cheeses like cheddar or Parmesan are less likely to trigger allergies because they have lower lactose content. Soft cheeses like Brie or blue cheese are more likely to cause issues due to higher lactose and mold content.
Not necessarily. A milk allergy is a reaction to milk proteins (casein or whey), while a cheese allergy could be specific to cheese proteins or additives. However, many cheese allergies are linked to milk proteins.
Yes, allergies can develop at any age. If you suddenly experience symptoms after eating cheese, it’s possible you’ve developed an allergy or intolerance. Consult an allergist for proper diagnosis.