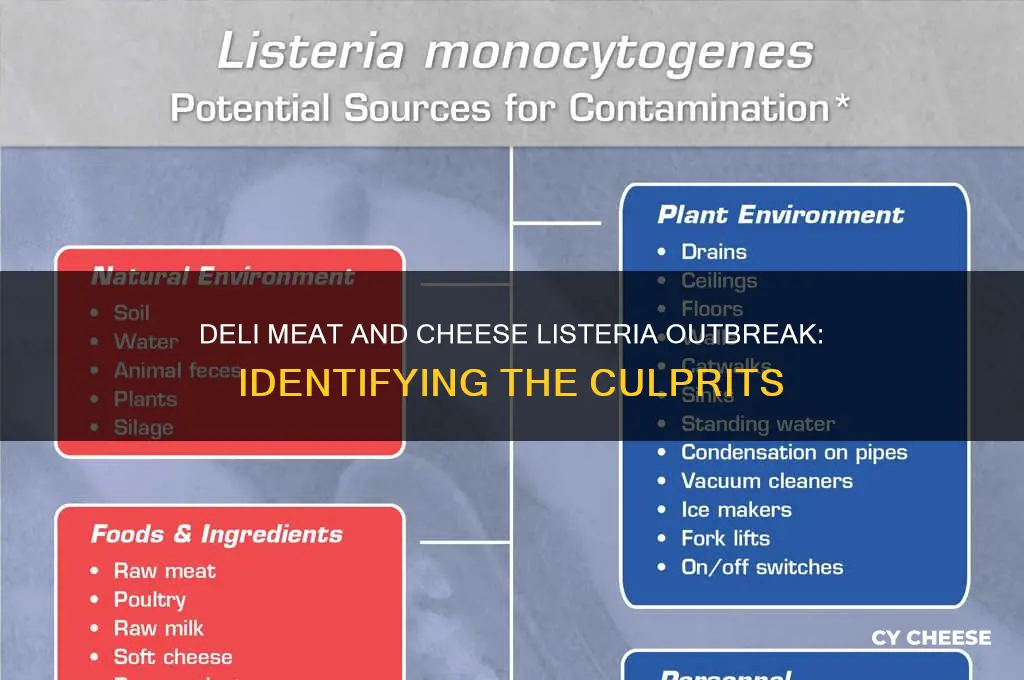
Recent outbreaks of listeria have raised concerns about the safety of certain deli meats and cheeses, prompting health authorities to investigate the sources of contamination. Listeria monocytogenes, the bacterium responsible for listeria infections, can thrive in ready-to-eat products like deli meats, hot dogs, and soft cheeses, particularly those stored in refrigerated conditions. Recent cases have been linked to specific brands and types of these products, with contaminated items often distributed across multiple states. Consumers are advised to check for recalls, practice proper food handling, and avoid high-risk products, especially pregnant women, the elderly, and those with weakened immune systems, who are most vulnerable to severe illness. Identifying the exact deli meats and cheeses causing these outbreaks is crucial for public health interventions and preventing further infections.
Explore related products
What You'll Learn

Deli Meat Brands Recalled
Recent recalls have spotlighted specific deli meat brands linked to Listeria outbreaks, raising urgent concerns for consumers. In October 2023, the USDA announced a recall of over 2,600 pounds of ready-to-eat meat and poultry products by New Jersey-based establishment, David’s Fine Foods, due to potential Listeria contamination. Similarly, in September 2023, Italian-style meats produced by Fratelli Beretta USA were recalled after samples tested positive for Listeria monocytogenes. These incidents underscore the vulnerability of processed meats to bacterial contamination, even in well-established brands.
Analyzing these recalls reveals common risk factors: improper handling during processing, cross-contamination in facilities, and inadequate refrigeration. Listeria thrives in cool environments, making deli meats particularly susceptible. Unlike other pathogens, it can grow at refrigerator temperatures, increasing the risk of infection even when products are stored correctly. Pregnant women, the elderly, and immunocompromised individuals are most at risk, with symptoms ranging from mild flu-like illness to severe complications like meningitis or miscarriage.
To protect yourself, follow these steps: First, check the USDA’s Food Safety and Inspection Service (FSIS) website regularly for updated recall lists. Second, inspect your refrigerator; ensure it’s set below 40°F (4°C) to slow bacterial growth. Third, separate deli meats from ready-to-eat foods to prevent cross-contamination. Finally, reheat deli meats to 165°F (74°C) before consumption, as this kills Listeria. While these measures reduce risk, they’re not foolproof—stay informed and act promptly if a recall affects products in your home.
Comparing recent recalls highlights a troubling trend: small-scale, localized outbreaks are increasingly common. Unlike large-scale recalls involving major brands, these incidents often fly under the radar, leaving consumers unaware. For instance, a 2022 recall of Mortadella by Columbus Foods affected only specific batch codes, yet the product was distributed nationwide. This disparity in visibility emphasizes the need for proactive consumer vigilance. Apps like FoodRecallWarning.org can help track recalls in real-time, ensuring you’re not caught off guard.
The takeaway is clear: no brand is immune to Listeria contamination. Even premium or organic labels can be affected, as processing conditions, not ingredients, are the primary risk factor. While recalls are a reactive measure, they serve as a critical reminder to prioritize food safety. By staying informed, practicing safe storage, and monitoring health advisories, consumers can mitigate risks associated with deli meats and cheeses. In an era of global supply chains, awareness is your best defense.
White Castle Cheese Sliders: Ingredients, Toppings, and Melty Magic Revealed
You may want to see also

Cheese Products Linked to Outbreaks
Recent outbreaks of listeria have spotlighted certain cheese products as culprits, raising concerns among consumers and health officials alike. Soft cheeses, such as Brie, Camembert, and queso fresco, have been frequently implicated due to their higher moisture content and lower acidity, which create an ideal environment for listeria growth. Pregnant women, the elderly, and individuals with weakened immune systems are particularly vulnerable, as listeria can cause severe complications, including miscarriage, sepsis, and meningitis. Understanding which cheeses pose risks is the first step in mitigating potential harm.
Analyzing the data reveals a pattern: unpasteurized or raw milk cheeses are more likely to harbor listeria than their pasteurized counterparts. For instance, a 2020 outbreak linked to Hispanic-style soft cheeses resulted in hospitalizations across multiple states. These cheeses, often made with raw milk, bypass the pasteurization process that kills harmful bacteria. Consumers should scrutinize labels for pasteurization status and avoid raw milk products if they fall into high-risk categories. Opting for hard cheeses like cheddar or Swiss, which are less hospitable to listeria, can be a safer alternative.
Instructive measures can significantly reduce the risk of listeria contamination from cheese. Always store cheese at or below 40°F (4°C) to slow bacterial growth, and consume soft cheeses within a week of opening. Thoroughly clean utensils and surfaces after handling cheese to prevent cross-contamination. For those preparing food for vulnerable populations, reheating soft cheeses until they are steaming can kill listeria. These simple steps, when consistently applied, can make a substantial difference in food safety.
Comparing the risks associated with different cheese types highlights the importance of informed choices. While soft, unpasteurized cheeses carry the highest risk, even pasteurized products can become contaminated during processing or handling. For example, a 2022 outbreak was traced back to a pasteurized brie contaminated post-production. This underscores the need for vigilance across all stages of cheese production and consumption. By staying informed about recalls and following safe handling practices, consumers can enjoy cheese while minimizing health risks.
Descriptive accounts of listeria outbreaks often reveal gaps in food safety protocols. In one case, a cheese manufacturer’s failure to sanitize equipment led to widespread contamination, affecting hundreds of products. Such incidents emphasize the critical role of regulatory oversight and industry compliance. Consumers can protect themselves by staying updated on recalls through the FDA’s website and reporting any suspected foodborne illnesses to local health departments. Awareness and proactive measures are key to preventing future outbreaks linked to cheese products.
Cutting Cheese Mold: How Many Inches to Safely Remove?
You may want to see also

Symptoms of Listeria Infection
Recent outbreaks have linked listeria contamination to deli meats like turkey, ham, and bologna, as well as soft cheeses such as Brie, Camembert, and queso fresco. These foods, often consumed without further cooking, provide an ideal environment for listeria to thrive. Understanding the symptoms of listeria infection is crucial for early detection and treatment, especially for vulnerable populations.
Recognizing the Onset of Listeria Symptoms
Symptoms typically appear 1 to 4 weeks after consuming contaminated food but can manifest as early as a few days or as late as 70 days. The initial signs often mimic mild flu: fever, muscle aches, fatigue, and sometimes gastrointestinal distress like nausea or diarrhea. These symptoms can be easily overlooked, but they are the body’s first warning of a potential listeria infection. If you’ve recently consumed deli meats or soft cheeses and experience these symptoms, monitor your condition closely.
Severe Symptoms and High-Risk Groups
While healthy individuals may experience only mild illness, listeria poses a serious threat to pregnant women, newborns, the elderly, and immunocompromised individuals. Pregnant women may suffer from headaches, stiff neck, confusion, loss of balance, or convulsions, which can lead to miscarriage, stillbirth, or premature delivery. Newborns infected during pregnancy may show signs of sepsis, such as difficulty breathing, lethargy, or poor feeding. For the elderly and immunocompromised, listeria can cause bloodstream infections (sepsis) or meningitis, requiring immediate medical attention.
Practical Steps for Monitoring and Response
If you suspect listeria infection, track your symptoms and note their severity. Mild cases may resolve on their own, but severe symptoms warrant urgent medical care. Pregnant women should seek medical advice at the first sign of illness, as prompt antibiotic treatment can prevent harm to the fetus. Keep a food diary to help identify potential sources of contamination, especially if others who consumed the same food also fall ill.
Preventive Measures to Reduce Risk
To minimize the risk of listeria infection, avoid consuming deli meats and soft cheeses unless they are thoroughly reheated to an internal temperature of 165°F (74°C). Store these foods at or below 40°F (4°C) and discard any products past their expiration date. Wash hands, utensils, and surfaces after handling deli meats or cheeses to prevent cross-contamination. For high-risk groups, consider avoiding these foods altogether or opting for safer alternatives like hard cheeses or freshly cooked meats. Early awareness and preventive actions can significantly reduce the likelihood of listeria infection.
Wood Pulp in Grated Cheese: Fact or Fiction?
You may want to see also
Explore related products
$8.99 $14.99
$7.99 $15.99

High-Risk Groups for Listeria
Pregnant women are among the most vulnerable to listeria infections, with a 10 to 20 times higher risk compared to the general population. The immune system changes during pregnancy make it easier for the bacteria to cross the placental barrier, potentially leading to miscarriage, stillbirth, or severe illness in newborns. A 2017-2018 outbreak linked to deli meats and cheeses resulted in one fetal loss and several hospitalizations, underscoring the critical need for caution. Pregnant women should avoid consuming deli meats and soft cheeses unless they are thoroughly heated to an internal temperature of 165°F (74°C) to kill the bacteria.
Individuals with weakened immune systems, such as those undergoing chemotherapy, living with HIV/AIDS, or taking immunosuppressive medications, face a significantly elevated risk of listeriosis. For example, organ transplant recipients are up to 500 times more likely to contract the infection. These individuals often lack the immune response necessary to combat listeria, allowing the bacteria to proliferate unchecked. Practical steps include avoiding high-risk foods like pre-packaged deli meats and opting for freshly sliced options, which have a lower contamination risk. Refrigerated foods should be consumed within four days to minimize bacterial growth.
Older adults, particularly those over 65, account for approximately 60% of listeriosis cases in the U.S. Age-related immune decline, known as immunosenescence, reduces the body’s ability to detect and destroy listeria. Chronic conditions like diabetes and liver disease, common in this demographic, further exacerbate vulnerability. To mitigate risk, seniors should inspect packaged deli meats and cheeses for expiration dates and avoid products past their prime. Reheating deli meats until steaming can also eliminate potential bacteria, though this may alter texture and flavor.
Infants and young children are at heightened risk due to underdeveloped immune systems. While listeriosis is rare in this group, it can be severe, leading to sepsis or meningitis. A 2019 outbreak linked to contaminated cheese products sickened several children under five, highlighting the importance of parental vigilance. Caregivers should avoid feeding infants soft cheeses or deli meats unless confirmed pasteurized and freshly prepared. Proper hand hygiene and food storage practices, such as keeping refrigerators below 40°F (4°C), are essential to prevent bacterial growth in household settings.
Does Classic Cheesecake Include Cinnamon? Unraveling the Ingredients Mystery
You may want to see also

Preventing Listeria Contamination
Recent outbreaks have linked Listeria monocytogenes to various deli meats and soft cheeses, particularly those stored improperly or past their prime. This bacterium thrives in cool, moist environments, making refrigerated, ready-to-eat products prime targets. While recalls help manage risks, prevention starts with understanding how Listeria infiltrates these foods and implementing targeted strategies to stop it.
Temperature Control: The Frontline Defense
Listeria grows between 39°F and 98.6°F, but it can survive refrigeration. Keep deli meats and cheeses at or below 40°F. Use appliance thermometers to verify fridge accuracy, as built-in gauges often misread by 5–10 degrees. For commercial settings, ensure display cases maintain consistent temperatures, especially during peak hours when doors open frequently. At home, store opened packages in airtight containers or vacuum-sealed bags to minimize exposure to warmer air.
Sanitization Practices: Beyond Surface-Level Cleanliness
Cross-contamination is a silent culprit. Listeria can linger on slicers, countertops, and utensils for weeks. Sanitize food-contact surfaces with a solution of 1 tablespoon unscented bleach per gallon of water, letting it air-dry to kill residual bacteria. Replace cutting boards and slicer blades annually, as scratches harbor microbes. In delis, implement color-coded equipment for raw and ready-to-eat items to prevent pathogen transfer.
Product Handling and Rotation: A Time-Sensitive Approach
Deli meats last 3–5 days in the fridge; soft cheeses like Brie or Camembert, 1–2 weeks. Use the “first in, first out” method, labeling packages with opening dates. Avoid bulk purchases unless freezing, as Listeria can grow even in chilled environments. For pregnant women, the elderly, or immunocompromised individuals, reheat deli meats to 165°F to eliminate potential bacteria, though this alters texture.
Industry and Regulatory Measures: Closing the Gaps
Manufacturers must adopt Hazard Analysis and Critical Control Points (HACCP) plans, monitoring processing steps like cooling and packaging. Post-production testing for Listeria is mandatory, with recalls triggered at 100 CFU/g in ready-to-eat meats. Retailers should segregate raw and cooked products, train staff in hygiene protocols, and discard items past expiration. Consumers should report suspicious products to the USDA or FDA, as recalls often stem from public alerts.
By combining vigilance at every stage—from factory to fridge—the risk of Listeria contamination in deli meats and cheeses can be significantly reduced, safeguarding public health without compromising convenience.
Calculating Cheese Weight: Pounds in 160 Slices Explained
You may want to see also
Frequently asked questions
Recent Listeria outbreaks have been associated with pre-packaged deli meats (such as ham, turkey, and roast beef) and soft cheeses (like Brie, Camembert, and Mexican-style cheeses like queso fresco). Always check for recalls and avoid consuming products past their expiration dates.
Listeria can contaminate deli meat and cheese through improper handling, cross-contamination during processing, or unsanitary conditions in production facilities. The bacteria can survive in refrigerated environments, making it a persistent risk in ready-to-eat products.
Pregnant women, newborns, the elderly, and individuals with weakened immune systems are most at risk. Symptoms include fever, muscle aches, nausea, and diarrhea. In severe cases, it can lead to miscarriage, stillbirth, or life-threatening infections like meningitis. Seek medical attention if symptoms occur after consuming suspect products.