The question of what a cheese-like smell from the vagina means is a common concern for many individuals, often prompting worry or confusion. This odor can stem from various factors, including bacterial imbalances, such as bacterial vaginosis, yeast infections, or poor hygiene. While a mild, musky scent is normal and healthy, a strong, cheesy odor may indicate an underlying issue that requires attention. Understanding the potential causes and seeking appropriate medical advice is crucial to maintaining vaginal health and addressing any discomfort or concerns.
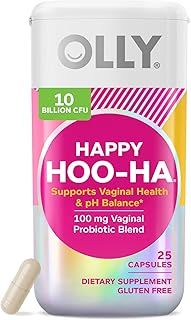
Explore related products
What You'll Learn
- Bacterial Vaginosis (BV): Overgrowth of bacteria causing fishy odor, often linked to pH imbalance
- Yeast Infections: Fungal overgrowth leading to bread-like or cheesy smell, with itching
- Poor Hygiene: Sweat, bacteria, and discharge buildup due to inadequate cleaning
- Dietary Impact: Strong-smelling foods like garlic or spices altering vaginal odor temporarily
- Hormonal Changes: Menstruation, pregnancy, or menopause affecting natural vaginal flora balance

Bacterial Vaginosis (BV): Overgrowth of bacteria causing fishy odor, often linked to pH imbalance
A vaginal odor resembling cheese can be a symptom of Bacterial Vaginosis (BV), a condition where the natural balance of bacteria in the vagina is disrupted. This imbalance often leads to an overgrowth of certain bacteria, producing a distinct fishy odor, especially after sexual intercourse or during menstruation. Understanding BV is crucial, as it is one of the most common vaginal infections, affecting women of all ages, particularly those in their reproductive years.
Identifying the Culprit: Gardnerella Vaginalis
BV is primarily associated with an overgrowth of *Gardnerella vaginalis*, a bacterium that thrives when the vagina’s pH rises above the normal range of 3.8 to 4.5. This shift creates an environment where harmful bacteria outcompete beneficial lactobacilli, which typically produce lactic acid to maintain acidity. The resulting odor is often described as "fishy" rather than cheesy, but the terms are sometimes used interchangeably due to the pungent nature of the smell. Key risk factors include douching, multiple sexual partners, and recent antibiotic use, which can disrupt the vaginal microbiome.
Symptoms and Diagnosis: Beyond the Odor
While the fishy odor is a hallmark of BV, other symptoms include thin, grayish-white discharge, itching, and a burning sensation during urination. However, up to 84% of women with BV are asymptomatic, making routine gynecological exams essential. Diagnosis involves a pelvic exam, pH testing (a pH above 4.5 is indicative), and a "whiff test," where adding potassium hydroxide to a sample of discharge amplifies the fishy smell. Laboratory tests may also identify clue cells—vaginal cells coated with bacteria—under a microscope.
Treatment and Prevention: Restoring Balance
BV is typically treated with antibiotics such as metronidazole (500 mg twice daily for 7 days) or clindamycin (300 mg twice daily for 7 days). These medications reduce bacterial overgrowth and restore pH balance. However, recurrence is common, with up to 30% of women experiencing symptoms within 3 months. Probiotics containing *Lactobacillus* strains can help maintain a healthy vaginal flora, and avoiding douching, scented hygiene products, and tight synthetic underwear reduces risk. Non-prescription boric acid suppositories (600 mg daily for 14 days) are an alternative for recurrent cases, though they should be used under medical supervision.
When to Seek Help: Red Flags and Complications
While BV is not a serious condition, untreated cases can lead to complications such as increased susceptibility to STIs, pelvic inflammatory disease, and adverse pregnancy outcomes like preterm birth. Women experiencing persistent symptoms despite treatment, severe pain, or fever should seek immediate medical attention. Pregnant individuals with BV require prompt treatment to minimize risks to the fetus. Regular check-ups and open communication with healthcare providers are vital for managing and preventing BV effectively.
Does Cheese Turn into Sugar? Unraveling the Body's Metabolic Mystery
You may want to see also

Yeast Infections: Fungal overgrowth leading to bread-like or cheesy smell, with itching
A cheesy or bread-like vaginal odor often signals a yeast infection, a common condition caused by an overgrowth of the fungus *Candida albicans*. This imbalance disrupts the vagina's natural microbiome, leading to symptoms like itching, irritation, and a thick, white discharge resembling cottage cheese. While yeast infections are not sexually transmitted, they can be triggered by factors like antibiotic use, hormonal changes, diabetes, or a weakened immune system.
Understanding the root cause is crucial for effective treatment and prevention.
Recognizing a yeast infection goes beyond the distinctive odor. The accompanying itching can range from mild discomfort to intense irritation, often worsening at night or after intercourse. Other symptoms include redness and swelling of the vulva, pain during urination or sex, and a burning sensation. It's important to note that these symptoms can overlap with other vaginal conditions, such as bacterial vaginosis or sexually transmitted infections. Therefore, accurate diagnosis is essential. Over-the-counter antifungal treatments, available as creams, ointments, or suppositories, are typically effective for mild to moderate cases. These medications, containing active ingredients like miconazole or clotrimazole, are applied vaginally for 3 to 7 days, depending on the product and severity of the infection.
For recurrent yeast infections (four or more per year), a healthcare provider may recommend a longer course of treatment or prescribe oral antifungal medication like fluconazole. Addressing underlying factors is equally important. This may involve managing blood sugar levels for diabetics, avoiding douching or scented products that disrupt vaginal flora, and wearing breathable cotton underwear. Probiotics, particularly those containing *Lactobacillus* strains, can help restore a healthy vaginal microbiome and reduce the risk of recurrence.
While yeast infections are generally not serious, untreated cases can lead to complications like severe discomfort or increased susceptibility to other infections.
Pregnant women and individuals with weakened immune systems should seek medical advice before using any treatment. Additionally, if symptoms persist despite treatment or are accompanied by fever, abdominal pain, or unusual discharge, consulting a healthcare professional is crucial to rule out more serious conditions. By understanding the causes, recognizing the symptoms, and seeking appropriate treatment, individuals can effectively manage yeast infections and maintain vaginal health.
Calculating 250g Cheese and Hamburger Cheese Quantities per Carton
You may want to see also

Poor Hygiene: Sweat, bacteria, and discharge buildup due to inadequate cleaning
A cheesy vaginal odor often signals poor hygiene, specifically the accumulation of sweat, bacteria, and discharge due to inadequate cleaning. This buildup creates an environment where bacteria thrive, producing volatile compounds like butyric acid—the same compound responsible for the pungent smell of aged cheese. Unlike occasional odor changes, which are normal, a persistent cheesy smell warrants attention.
Understanding the Culprits:
Sweat from the groin area, combined with natural vaginal discharge, provides a moist breeding ground for bacteria. When not regularly cleansed, these substances accumulate, especially in skin folds or tight clothing. Bacteria break down proteins in sweat and discharge, releasing gases that contribute to the odor. Poor hygiene exacerbates this process, as leftover menstrual blood, urine, or fecal matter can further feed bacterial growth.
Practical Steps to Address the Issue:
To mitigate this odor, adopt a gentle yet consistent cleaning routine. Wash the external vaginal area daily with warm water and a fragrance-free, pH-balanced cleanser. Avoid douching, as it disrupts natural flora and can worsen odor. Change underwear daily, opting for breathable fabrics like cotton. After sweating or exercise, shower promptly to remove moisture and bacteria. For post-menstrual or post-bowel movement hygiene, wipe front to back to prevent bacterial transfer.
Cautions and Considerations:
Over-cleansing or using harsh soaps can strip the vagina’s protective pH, leading to irritation or infections like bacterial vaginosis, which also causes a cheesy odor. Avoid scented products, talcum powders, or tight synthetic clothing, as these trap moisture and irritate skin. If odor persists despite proper hygiene, consult a healthcare provider to rule out underlying conditions like infections or hormonal imbalances.
Takeaway:
Poor hygiene is a reversible cause of a cheesy vaginal odor. By maintaining a balanced cleaning routine, wearing breathable fabrics, and addressing moisture promptly, most individuals can eliminate this issue. However, persistent odor despite these measures may indicate a health concern requiring professional evaluation.
Arby's Ham and Cheese Sliders: Are They Still on the Menu?
You may want to see also
Explore related products

Dietary Impact: Strong-smelling foods like garlic or spices altering vaginal odor temporarily
The foods we consume can have a surprising impact on our bodies, and this extends to vaginal odor. Strong-smelling foods like garlic, onions, and certain spices contain volatile compounds that are excreted through sweat, urine, and even vaginal secretions. This means that indulging in a garlicky pasta dish or a spicy curry can temporarily alter the scent of your vagina.
Understanding the Mechanism:
When you eat foods with potent aromas, their sulfur-containing compounds, like allicin in garlic, are metabolized and released into your bloodstream. These compounds then travel throughout your body, eventually reaching the sweat glands and mucous membranes, including those in the vaginal area. This process can lead to a noticeable change in vaginal odor, often described as "cheesy" or "musky," within a few hours of consumption.
Temporary Nature:
It's crucial to emphasize that these dietary-induced odor changes are temporary. The scent typically dissipates within 24-48 hours as your body eliminates the compounds. This means that while a garlic-heavy meal might lead to a temporary shift in vaginal odor, it's not a cause for concern and doesn't indicate an underlying health issue.
Practical Considerations:
If you're concerned about the impact of strong-smelling foods on your vaginal odor, consider moderating your intake, especially before intimate encounters. However, it's important to remember that everyone's body is different, and what causes a noticeable change in one person may not have the same effect on another. Experimenting with your diet and observing your body's response can help you understand your individual sensitivities.
Embracing Natural Variation:
Vaginal odor is a natural and normal part of a woman's body, and it can fluctuate due to various factors, including diet, hormonal changes, and menstrual cycle. While strong-smelling foods can temporarily alter this odor, it's essential to embrace the natural variations and not feel pressured to conform to a specific scent. A healthy vagina has a unique, individual scent that is perfectly normal and should be celebrated. If you notice a persistent, strong, or unpleasant odor accompanied by other symptoms like itching, burning, or discharge, consult a healthcare professional to rule out any underlying infections or conditions.
Essential Tools and Tips to Launch Your Cheese Making Business
You may want to see also

Hormonal Changes: Menstruation, pregnancy, or menopause affecting natural vaginal flora balance
Vaginal odor often reflects the delicate balance of its microbiome, influenced heavily by hormonal fluctuations. During menstruation, pregnancy, or menopause, estrogen and progesterone levels shift, altering vaginal pH and glycogen production. This creates an environment where certain bacteria thrive, sometimes producing a scent reminiscent of cheese. Understanding these hormonal changes can demystify the odor and guide appropriate responses.
Consider menstruation: blood and tissue shedding during this phase introduce foreign substances to the vagina, temporarily disrupting its flora. The pH rises from its typical acidic state (around 3.8–4.5) to a more neutral level, favoring the growth of bacteria like *Gardnerella vaginalis*. This shift can result in a mild, cheesy odor, often accompanied by a thin, grayish discharge—a condition known as bacterial vaginosis (BV). While BV is common during menstruation, it’s usually harmless and resolves post-period. However, persistent symptoms warrant a healthcare consultation to rule out infection.
Pregnancy amplifies hormonal changes, with elevated estrogen levels increasing vaginal glycogen. This fuels the growth of lactobacilli, which maintain acidity and protect against pathogens. Yet, hormonal surges can also lead to excessive discharge (leukorrhea), sometimes with a mild, cheesy scent. This is generally normal, but a sudden change in odor, color, or consistency could indicate an infection like yeast overgrowth or BV, which require medical attention to prevent complications like preterm birth.
Menopause, marked by estrogen decline, reduces vaginal glycogen and lactobacilli, raising pH levels. This shift often results in a drier, thinner vaginal lining, a condition called vaginal atrophy. The altered flora can produce a musty or cheesy odor, accompanied by itching or discomfort. Over-the-counter vaginal moisturizers or estrogen creams (0.5–1g applied twice weekly) can restore balance, but consult a healthcare provider for personalized advice.
Practical tips for managing hormonal-related odors include wearing breathable cotton underwear, avoiding scented hygiene products, and practicing gentle cleansing with water. Probiotic supplements containing *Lactobacillus rhamnosus* GR-1 and *L. reuteri* RC-14 (10 billion CFU daily) may support flora balance during menstruation or menopause. However, persistent or severe symptoms—such as burning, itching, or foul-smelling discharge—require medical evaluation to differentiate between normal hormonal effects and treatable conditions.
Annual Sales of Iconic Cheesehead Hats: A Surprising Figure Revealed
You may want to see also
Frequently asked questions
A cheese-like smell from the vagina is often due to bacterial vaginosis (BV), an imbalance of vaginal bacteria, or a buildup of sweat and bacteria in the genital area.
Not always. A mild, musky, or slightly cheesy odor can be normal due to hormonal changes, sweat, or natural vaginal flora. However, a strong or persistent odor may indicate an infection like BV or a yeast infection.
If the smell is accompanied by symptoms like itching, burning, unusual discharge, or discomfort, it’s best to consult a healthcare provider. These could be signs of an infection that requires treatment.
Yes, diet (e.g., spicy foods, dairy) and poor hygiene can contribute to changes in vaginal odor. Wearing tight clothing or not changing out of sweaty clothes promptly can also lead to bacterial growth and a cheesy smell.