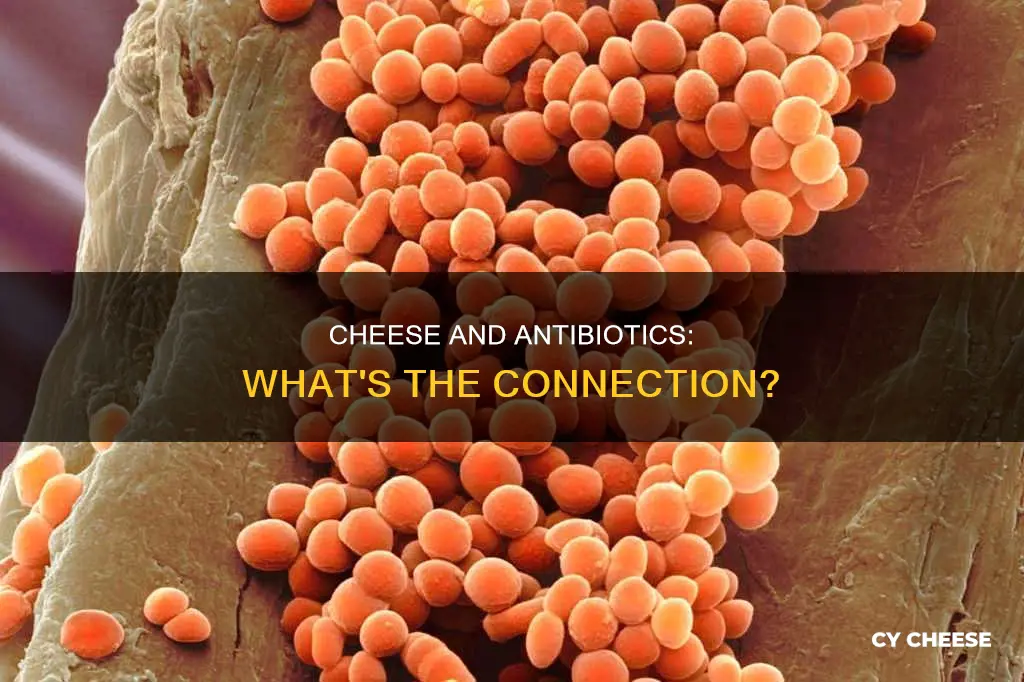
The presence of antibiotics in cheese is a topic of interest in the scientific community. While some studies focus on the antibiotic properties of certain types of cheese, such as blue cheese, others explore the impact of antibiotic-resistant bacteria in cheese fermentation and the potential health risks associated with it. The diversity and abundance of antibiotic resistance genes (ARGs) in cheese can vary, and the consumption of cheese containing these genes is a concern for food safety and public health. Additionally, the influence of fungal antibiotics on microbiome development in cheese has also been investigated, providing insights into the complex microbial communities present in cheese rinds.
| Characteristics | Values |
|---|---|
| Are any types of cheese antibiotic? | No, but some cheeses contain antibiotic-resistant bacteria and antibiotic-resistant genes. |
| Which types of cheese contain antibiotic-resistant bacteria and genes? | Commercially produced cheeses sold in China, Swiss cheese, and retail cheese samples from the US. |
| Which bacteria and genes were found in the cheese? | Streptococcus, Lactococcus, Lactobacillus, Staphylococcus, Leuconostoc, and antibiotic-resistant genes (ARGs). |
| Are blue cheese and penicillin related? | Blue cheese contains cultures of Penicillium mould, but the strains used in cheesemaking are different from those used in penicillin and don't have significant antibiotic properties. |
Explore related products
What You'll Learn

Blue cheese and antibiotic resistance
Blue cheese is manufactured with a variety of the Penicillium mould, which was discovered by Alexander Fleming in 1928 to have antibiotic properties. The antibiotic properties of penicillin, derived from a species of Penicillium fungus, are still widely used today, although many bacteria have become resistant to the drug over time.
Antibiotic resistance occurs when bacteria are regularly exposed to doses of antibiotics that are not strong enough to kill all the bacteria. This results in only the weakest bacteria being killed off, leaving the slightly stronger ones to multiply and spread their more resistant genes.
Given that blue cheese contains cultures of Penicillium mould, one might assume that consuming excessive amounts of blue cheese could contribute to antibiotic resistance by overexposing the bacteria in the body to Penicillium. However, it is important to note that the strains of Penicillium used in cheesemaking differ from those used in antibiotics. Moreover, these strains lack significant antibiotic properties and are destroyed by stomach acid.
The main cheese-making Penicilliums, including roqueforti (blue cheese), camemberti (Camembert and Brie), and glaucum (Gorgonzola), do not produce penicillin. While they do produce other antibacterial metabolites, as well as human toxins and allergens, they do not yield any medically useful antibiotics.
In conclusion, while blue cheese does contain Penicillium mould, the specific strains used in cheesemaking lack significant antibiotic properties. Therefore, consuming blue cheese is unlikely to contribute to antibiotic resistance.
The Cheddar Cheese Family: How Big Is It?
You may want to see also

Antibiotic-resistant bacteria in cheese
Antibiotic resistance is a major public health concern. Bacteria develop resistance when they are regularly exposed to doses of antibiotics that are not strong enough to kill them. This leaves only the slightly stronger bacteria to multiply and spread their more resistant genes.
Cheese is a potential source of antibiotic-resistant bacteria, with a variety of antibiotic-resistant genes (ARGs) found in commercially produced cheeses. A study on cheese produced in China found that Lactococcus, Lactobacillus, and Streptococcus were the dominant bacteria in the cheese samples. Multidrug-resistant lactic acid bacteria were isolated from most types of cheese, with 100% and 91.7% of isolates resistant to streptomycin and sulfamethoxazole, respectively. The occurrence and abundance of ARGs varied significantly between the 15 cheeses studied.
Another study examined Cheddar-type cheeses and found that with proper sanitation controls, the production of antibiotic-resistant-bacterium-free cheese is achievable. However, the presence of antibiotic-resistant bacteria in cheese fermentation is a concern for food safety and public health. The study also investigated the prevalence of antibiotic-resistant bacteria in retail cheese samples and found a reduction in the prevalence of antibiotic resistance in samples from 2010 compared to 2006, suggesting the effectiveness of targeted antibiotic resistance mitigation strategies.
It is important to note that the strains of Penicillium mould found in blue cheese are different from those used to derive penicillin and do not possess significant antibiotic properties. Additionally, these moulds are destroyed by stomach acid.
Overall, while cheese can contain antibiotic-resistant bacteria, the risks associated with consumption are mitigated by proper sanitation controls and the action of stomach acid. However, further research and targeted mitigation strategies are necessary to address the presence of antibiotic-resistant bacteria in cheese and prevent potential food safety and public health issues.
Healthy Cheeses: Nutritional Benefits and Varieties
You may want to see also

Cheese and human health
Cheese is a beloved food product worldwide, but it also has an impact on human health. The presence of antibiotic-resistant bacteria in cheese is a growing concern, especially with the rise of antibiotic resistance in bacteria.
Antibiotic Resistance in Cheese
Cheese can be a source of antibiotic-resistant bacteria, which has been a major public health concern. A study in 2011 found high levels of antibiotic-resistant bacteria and a representative antibiotic resistance (AR) gene pool in most cheese samples examined, including various types and brands. The presence of AR genes in cheese products and the identification of certain isolates carrying AR genes as lactic acid bacteria raised concerns about the potential impact of the dairy fermentation process on the emergence and amplification of antibiotic-resistant bacteria.
Impact on Human Health
The consumption of cheese containing antibiotic-resistant bacteria can have potential implications for human health. The AR genes from food-borne isolates can be transmitted to human-pathogenic and residential bacteria, leading to acquired resistance in the recipient cells. This suggests the functionality and mobility of food-borne AR genes. The transmission of AR genes can occur through horizontal gene transfer (HGT) mechanisms, which is a concern as lactic acid bacteria are prone to HGT events.
Mitigation Strategies
To address the issue of antibiotic resistance in cheese, targeted mitigation strategies have been implemented by the dairy and starter culture industries. These efforts have shown some success, as there has been a reduction in the prevalence of AR in retail cheese products. Proper sanitation controls and pasteurization are also crucial in producing cheese that is free of antibiotic-resistant bacteria.
Fungal Antibiotics in Cheese
In addition to bacterial cultures, fungi present in cheese, such as the Penicillium mold in blue cheese, can also have an impact on human health. While the strains of Penicillium used in cheesemaking do not possess significant antibiotic properties, studies have shown that fungal antibiotics can influence microbiome development. This indicates that the antibiotics secreted by fungi can control how microbiomes develop, not only in cheese but also in other ecosystems, including the human microbiome.
Overall Impact
The presence of antibiotic-resistant bacteria and the transmission of AR genes through cheese consumption can contribute to the broader issue of antibiotic resistance. While there have been efforts to mitigate this issue, it is important to continuously monitor and address the presence of antibiotic-resistant bacteria in cheese to ensure food safety and protect public health.
Babybel Cheese: A Comprehensive Guide to Its Kinds
You may want to see also
Explore related products

Fungal antibiotics in cheese
Cheese rinds are microbial communities that form on the surfaces of naturally aged cheeses such as Brie, Taleggio, and some Cheddars. The fuzzy and sometimes sticky layers on the surfaces of these cheeses are communities of microbes that develop as the cheese is aged. They slowly decompose the cheese curd as they grow on the surface and produce aromas and pigments that give each artisan cheese unique properties.
Cheese rinds are a perfect playground for studying fungal antibiotics. Fungi produce metabolites that humans have used to improve health. For example, they secrete penicillin, which is then purified and used as an antibiotic for humans, leading to the development of many other antibiotics. However, the ecology of fungal metabolites in microbial communities is not well understood.
In a study published in the journal mBio, researchers used cheese rinds to demonstrate that fungal antibiotics can influence how microbiomes develop. They found that antibiotics secreted by fungi can control how microbiomes develop. The study was conducted by Benjamin Wolfe, PhD, associate professor in the Department of Biology at Tufts University, and his team.
Wolfe and his team began by investigating a cheesemaker’s problem with mold spreading on the surface of the cheeses and disrupting the normal development of the rind. They collaborated with Nancy Keller's lab at the University of Wisconsin to find out what this mold was doing to the rind microbes and what chemicals the mold may be producing that disrupted the rind.
They first deleted a gene (laeA) in the Penicillium mold that is known to control the expression of chemicals that fungi can secrete into their environment. These compounds are called specialized or secondary metabolites. When laeA was deleted, most of the antibacterial activity of the Penicillium mold was lost. This discovery helped the team narrow down specific regions of the fungal genome that could produce antibacterial compounds. They narrowed it down to one class of compounds called pseurotins. The metabolites are produced by multiple types of fungi and that can modulate the immune system, kill insects, and inhibit bacteria.
The study showed that pseurotins can also control how bacterial communities living with that fungi grow and develop. The pseurotins are strongly antibacterial, which means they inhibit some of the bacteria found in artisanal cheeses including Staphylococcus, Brevibacterium, Brachybacterium, and Psychrobacter. This process caused a shift in the cheese rind microbiome’s composition.
It also shows that the antibiotics secreted by fungi can control how microbiomes develop, since the metabolites are in other ecosystems, including the human microbiome and soil ecosystems. The team expects that these mechanisms of fungal-bacterial interactions are likely very widespread.
The Mystery of Red Babybell: What Cheese is it?
You may want to see also

Antibiotics in mould-ripened cheese
While it is true that fungi produce metabolites that have been used to improve human health, including penicillin, the presence of antibiotics in mould-ripened cheese is a more complex issue. The ecology of fungal metabolites in microbial communities is not yet fully understood, and recent studies have shed light on the influence of fungal antibiotics on microbiome development.
Cheese rinds, such as those found on Brie, Taleggio, and some Cheddars, are microbial communities that form on the surfaces of naturally aged cheeses. These fuzzy layers are composed of microbes that develop and slowly decompose the cheese curd as the cheese ages. They also produce unique aromas and pigments that give each artisanal cheese distinct characteristics.
In a study conducted by Benjamin Wolfe, PhD, and colleagues at Tufts University, the impact of fungal antibiotics on microbiome development was investigated using cheese rinds as a model microbial ecosystem. They collaborated with Nancy Keller's lab at the University of Wisconsin to study the ecology, genetics, and chemistry of fungal-bacterial interactions, specifically focusing on the Penicillium mould. By deleting a gene (laeA) known to control the expression of chemicals secreted by fungi, they discovered that the antibacterial activity of the Penicillium mould was significantly reduced. This led them to identify one class of compounds called pseurotins, which are produced by a range of fungi and have various biological activities, including antibacterial properties.
The study revealed that antibiotics secreted by fungi can indeed influence the development of microbiomes. It also suggested that certain mould species in artisan cheeses may hinder normal cheese development by producing antibiotics. However, it's important to note that the strains of Penicillium used in cheesemaking differ from those used in penicillin production and do not possess significant antibiotic properties. Additionally, they are destroyed by stomach acid, as mentioned in a BBC Science Focus Magazine article.
Furthermore, a 1965 research article in the Journal of Dairy Science explored the possibility of penicillin production in commercial blue mould-ripened cheese. The study found that while no penicillin production was observed, over 60% of the analysed Blue and Roquefort cheeses exhibited penicillinase-like activity, indicating that these cheeses may be beneficial to penicillin-sensitive individuals.
In summary, while mould-ripened cheeses can contain antibiotics, the specific strains of Penicillium used in cheesemaking may not have significant antibiotic properties. Further research is needed to fully understand the complex interactions between fungi, bacteria, and the development of microbial communities in cheese.
The Best Cheeses for a Grilled Cheese Sandwich
You may want to see also
Frequently asked questions
No kind of cheese is an antibiotic, but some cheeses do contain antibiotic properties.
Blue cheese, for example, contains cultures of Penicillium mould, which has antibiotic properties.
Yes, several other cheeses such as Brie, Taleggio, and some Cheddars also contain antibiotic properties due to the presence of fungal antibiotics in their rinds.
While some cheeses do contain antibiotic properties, the specific strains of Penicillium used in cheesemaking lack significant antibiotic properties and are destroyed by stomach acid. Therefore, consuming cheese is unlikely to contribute to antibiotic resistance.